Improving DRG Based Reimbursement to Reflect Complexity of Kidney Transplant
1Surgery, University of Iowa, Iowa City, IA, 2Saint Louis University, St. Louis, MO, 3Surgery, Universtiy of Iowa, Iowa City, IA
Meeting: 2020 American Transplant Congress
Abstract number: 436
Keywords: Donors, marginal, Economics, Kidney transplantation, Resource utilization
Session Information
Session Time: 9:59am-10:40am
 Presentation Time: 10:30am-10:37am
Presentation Time: 10:30am-10:37am
Location: Main Channel
*Purpose: More than 90,000 individuals await a kidney transplant (KTx) in the US, yet up to 20% of recovered kidneys are discarded. Organ Transplant Centers have been challenged by the Executive Order to increase access by accepting patients with more comorbidities and using higher-risk organs. However, there have been no corresponding modifications to the Medicare reimbursement policies. While other transplant diagnosis related groups include adjustments for major complicating comorbidity (MCC), KTx does not. In this single center study, we apply Medicare ICD10 criteria to KTx to assess the prevalence of MCCs and their impact on cost.
*Methods: Isolated KTx patients at the University of Iowa between 10/2015 and 10/2019 were reviewed to assess the prevalence of MCCs. The need for post-transplant dialysis was NOT considered as an MCC. Donor and recipient characteristics associated with MCCs were determined.. Associations were analyzed with regression analysis and independent sample t-tests. Potential incremental revenue resulting from creation of a DRG with MCC was determined by applying the payment ratio for liver transplant with and without MCC to KTx.
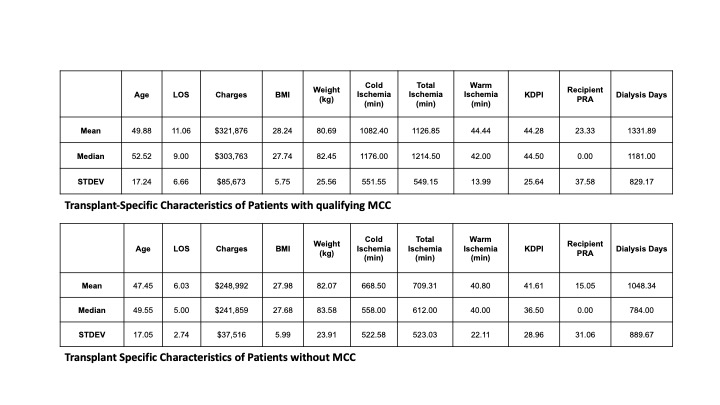
*Results: Among 270 KTx recipients, 52 (19%) had a condition that would have qualified as an MCC. Patients with MCCs had been waiting nearly a year longer for a transplant. (1332 days v 1048 days, p<0.001) and had a higher incidence of delayed graft function 42% vs 6% than non KTx without MCC cases (p<0.001). There were no differences in recipient age, gender, race, or diagnosis. Donor Factors correlated with MCC include greater total ischemic time (1127 min. vs 709 min., p<0.001) and cold ischemic time (1082 min. v. 669 min., p<0.001). There was no significant relationship between MCCs and kidney donor profile index among deceased onors (p=0.576), however, significantly fewer KTx with MCC received living donor KTx (9% vs. 32%, P<.001). Billed charges for KTx with MCCs were 29% higher ($321,876 vs. $248,992, p<0.001). KTx with MCC was associated with a longer length of stay (11.1 days vs. 6.03days, p<..001). Applying similar payment ratios for KTx with MCCs as in liver and heart transplant, a DRG with MCC would have increased overall revenue by $2.1 million over the last 4 years.
*Conclusions: This study demonstrates that the current Medicare guidelines for major complicating comorbidities are associated with higher cost kidney transplants, illustrating the need for a second DRG in kidney transplantation that reflects the complications of using these organs.
To cite this abstract in AMA style:
Schwantes IR, Schnitzler M, Lentine K, Reed A, Axelrod DA. Improving DRG Based Reimbursement to Reflect Complexity of Kidney Transplant [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/improving-drg-based-reimbursement-to-reflect-complexity-of-kidney-transplant/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress