Impact of Recipient Body Mass Index in Short and Long Term Survival of Pancreatic Grafts
Division of Visceral and Transplantation Surgery, University Hospitals of Geneva, Geneva, Switzerland
Division of Clinical Epidemiology, University Hospitals of Geneva, Geneva, Switzerland
Meeting: 2013 American Transplant Congress
Abstract number: 397
Background: In pancreas transplantation, the impact of recipient BMI on short and long term pancreas graft survival has not been studied.
Methods: We analyzed data from all individuals who underwent a first pancreas transplant from Oct. 1, 1987 to Aug. 30, 2011 and recorded in the Scientific Registry of Transplant Recipients. Recipients were categorized into BMI classes, as defined by WHO. Long-term graft failure was defined as return to insulin therapy and therefore includes post-transplant diabetes mellitus (PTDM). Patient and graft survival were analyzed by Kaplan-Meyer.
Results: 21,075 individuals were included in the analysis. Median follow-up was 4 years. Subjects were overweight or obese in 39%. Early pancreas graft loss increased with recipient BMI (p<.001).
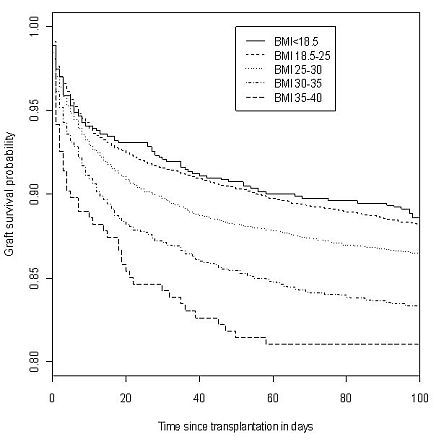
Compared to normal or low BMI, risk of early graft failure at 90 days increased by 21%, 50% and 74%, for overweight, obese class I and obese class II recipients, respectively. Early mortality was similar in all groups, except for class II obese recipients in whom risk of death increased by 84% as compared to other groups. Compared to normal or overweight BMI, risk of graft failure at 4 years increased by 23%, 15% and 35%, for underweight, obese class I and obese class II recipients, respectively. The low graft survival in underweight recipients (Figure 2) was associated with a risk of death increased by 67% as compared to normal BMI recipients at 4 years.
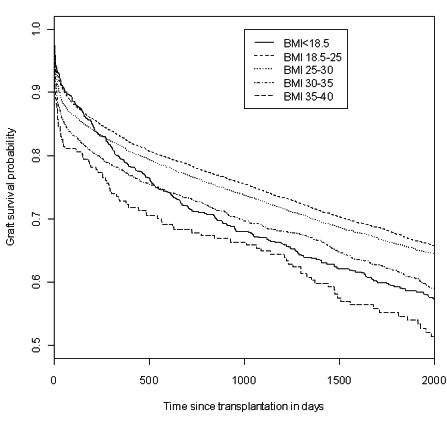
Conclusion: Increased BMI is associated with an increased risk of early graft loss and early mortality. Increased BMI does not seem to be associated with an increased incidence of PTDM. BMI (<18.5) is associated with an increased risk of death in the long term.
To cite this abstract in AMA style:
Bédat B, Niclauss N, Andres A, Jannot A, Toso C, Morel P, Berney T. Impact of Recipient Body Mass Index in Short and Long Term Survival of Pancreatic Grafts [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/impact-of-recipient-body-mass-index-in-short-and-long-term-survival-of-pancreatic-grafts/. Accessed February 16, 2026.« Back to 2013 American Transplant Congress
