Impact of Recipient BMI: Implications for ECD Renal Transplantation
Surgery, Duke University, Durham, NC
Meeting: 2013 American Transplant Congress
Abstract number: 534
Introduction: Donor and recipient obesity appear to be independent risk factors for renal graft failure (GF). In the ECD context, this additional risk might increase GF. Analysis of this risk could help improve recipient selection for ECD organs.
Objective:To evaluate impact of donor and recipient BMI (kg/m2) and donor terminal creatinine (RF) on risk of GF following transplantation among ECD vs SCD kidneys.
Methods: Adults deceased donor renal recipients in the OPTN/UNOS database between 2002 & 2010 were eligible. Donor GFR was estimated by MDRD equation and grouped by CKD stage. Donor & recipient BMI were grouped as: <25, 25-29, 30-34,≥35. Impact of donor & recipient BMI and donor RF on risk of GF and death-censored graft loss (DCGL) was assessed using Cox proportional hazards model. Effect modification was assessed by relevant two-way interactions in the Cox model.
Results: 54,600 patients with donor CKD stage 1, 2 or 3 were included (22% ECD). Kaplan-Meier GS at 4-years was 75%. Results of the multivariable analysis are provided in Table 1. Donor & recipient BMI and donor CKD stage were independently associated with increased GF and DCGL (two-way interactions with ECD vs. SCD not significant). The incremental impact of recipient BMI on the risk of DCGL observed with ECD kidneys is presented in Figure 1. For ECD recipients with BMI ≥ 35, the risk of DCGL is nearly 2.5 times that of a recipient whose BMI is < 25 who receives a SCD kidney.

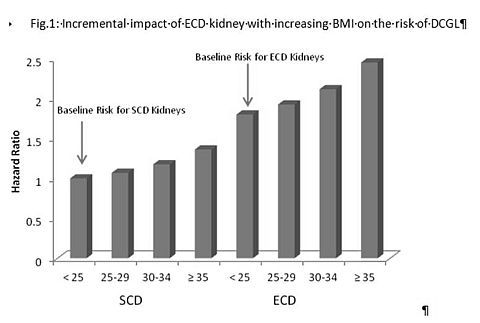
Conclusions: Donor & recipient BMI and donor RF are independently associated with increased risk of GL and DCGL.Their effect compounds the risk already associated with ECD kidneys. Strategies to improve ECD graft survival might include preferential use of these kidneys in non-obese recipients and emphasize weight reduction in wait list patients who are deemed candidates for ECD.
To cite this abstract in AMA style:
Ravindra K, Irish W, Vikraman D, Castleberry A, Barbas A, Sanoff S, Patel U, Ellis M, Sudan D. Impact of Recipient BMI: Implications for ECD Renal Transplantation [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/impact-of-recipient-bmi-implications-for-ecd-renal-transplantation/. Accessed February 27, 2026.« Back to 2013 American Transplant Congress
