Impact of Rapid Discontinuation of Prednisone on Kidney Transplant Outcomes in At-Risk Subpopulations: An OPTN/SRTR Analysis
1Public Health, U of MN, Mpls, MN
2Surgery, U of MN, Mpls, MN.
Meeting: 2018 American Transplant Congress
Abstract number: 432
Keywords: Immunosuppression, Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Immunosuppression: General Considerations - 1
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:42pm-2:54pm
Presentation Time: 2:42pm-2:54pm
Location: Room 6C
Objective: Successful RDP (rapid discontinuation of prednisone <1 week post-tx) after kidney transplant (KTx) has been reported for low-risk populations. We studied the impact of RDP in KTx subpopulations thought to be at increased risk.
Methods: Using SRTR data, we studied patient survival (PS) and death-censored graft survival (DCGS) in 1st and 2nd KTx-alone recipients between 1/1/2000-12/31/2014 with follow-up through 6/30/2016. We defined RDP based on the maintenance immunosuppression (MIS) at discharge. We restricted analysis to those with typical induction (IL2 inhibitors, thymoglobulin, or none) and maintenance IS (TAC + MMF or CSA + MMF) during the study. To assess the effect of RDP, we fit mixed-effect Cox proportional hazards models adjusting for IS regimen, recipient (age, race, gender, BMI, functional status, pre-tx dialysis, primary disease, diabetes [y/n], peak PRA), donor (age, race, HTN [y/n], creatinine, cause of death, DBD vs DCD, HLA mm), and surgical (ischemic time, date tx) characteristics. Transplant center was included as a random effect. Separate models were fit for each subgroup of interest (e.g., African American (Afr Am), obese, highly sensitive, 2nd KTx, and pediatric recipients) and for deceased and living donors.
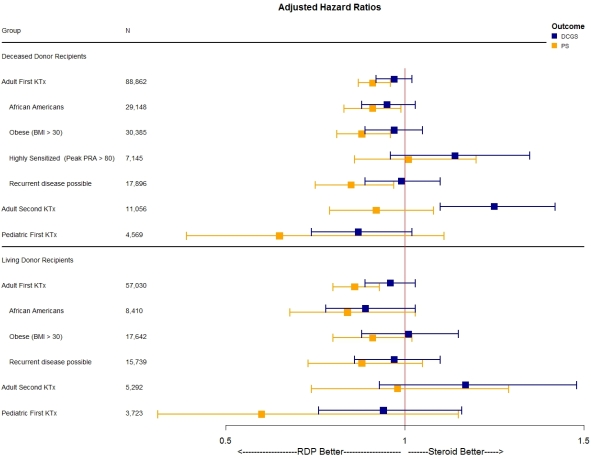
Results: 171,279 KTx (25.9% RDP) met inclusion criteria. RDP use increased from 3.1% in 2000 to 30.3% in 2014. Figure 1 gives the adjusted hazard ratios comparing RDP versus steroid use. Across all subgroups of 1st KTx recipients, there was no significant association of RDP on DCGS; furthermore, RDP was associated with a significantly decreased hazard of death for recipients of DD KTx for Afr Am (HR = 0.91), the obese (HR = 0.88) and those with a primary disease which could re-occur in the transplanted kidney (HR = 0.85) with similar trends for recipients of LD KTx. However, in 2nd DD KTx (but not 2nd LD KTx) RDP was associated with a higher hazard of DC graft failure (HR = 1.25), with no significant difference in PS.
Conclusion: RDP may be used across a wide range of subpopulations of 1st KTx recipients without risk of increased graft loss.
Figure 1: Comparison of steroid use for DCGS and PS by subgroups.
CITATION INFORMATION: Vock D., Matas A. Impact of Rapid Discontinuation of Prednisone on Kidney Transplant Outcomes in At-Risk Subpopulations: An OPTN/SRTR Analysis Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Vock D, Matas A. Impact of Rapid Discontinuation of Prednisone on Kidney Transplant Outcomes in At-Risk Subpopulations: An OPTN/SRTR Analysis [abstract]. https://atcmeetingabstracts.com/abstract/impact-of-rapid-discontinuation-of-prednisone-on-kidney-transplant-outcomes-in-at-risk-subpopulations-an-optn-srtr-analysis/. Accessed February 19, 2026.« Back to 2018 American Transplant Congress