Impact of Pre-Existing Comorbidities on Long-Term Patient and Graft Survival in Kidney Transplant Recipients.
Nephrology, Charité
University, Berlin, Germany.
Meeting: 2016 American Transplant Congress
Abstract number: A259
Keywords: Kidney transplantation, Outcome, Survival
Session Information
Session Name: Poster Session A: Poster Session III: Kidney Complications-Other
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
BACKGROUND Outcomes of patients with end-stage renal disease are largely affected by their comorbidities. Detailed data evaluating the impact of pre-transplant comorbidities on the long-term outcome after kidney transplantation are missing.
METHODS In a long-term retrospective analysis we investigated 878 deceased donor kidney transplant recipients (KTR) transplanted 1996-2014. Comorbidities at time of transplantation were diligently determined. Influences of pre-existing coronary artery disease (CAD), diabetes mellitus type 2 (DM), peripheral artery disease (PAD), chronic heart failure (CHF) and cerebrovascular disease (CVD) on outcomes were assessed. Kaplan-Meier and Cox regression analysis were performed to determine predictors of patient and graft survival.
RESULTS The mean age was 53 years and mean follow-up was 5.8 years. Prevalence of comorbidities at time of transplantation was: CAD 25%, DM 16%, PAD 11%, CHF 8% and CVD 7%. KTR with pre-existing CAD, DM, PAD and CHF showed a significantly poorer patient survival (Fig. 1a-b+d-e). Pre-existing CVD did not correlate with an elevated mortality. (Fig 1f). Multivariate analysis adjusting for all relevant factors and comorbidities identified only CAD and DM as independent risk factors for death (HR 1.77; p<0.001 and HR 1.53; p=0.016). KTR with both of these comorbidities showed superimposed mortality (48% after 7 years). Other independent risk factors for death were HLA-mismatches and cold ischemia time (HR 1.12; p=0.015 and HR 1.34; p=0.025).
A multivariate analysis of all examined comorbidities revealed CHF and PAD as independent risk factors for death censored graft loss (HR 2.23; p=0.003 and HR 1.70; p=0.028). Other independent risk factors were donor age (HR 1.20; p=0.009) and HLA-mismatches (HR 1.23; p<0.001).
CONCLUSION Pre-existing CAD and DM are independent risk factors predicting mortality in KTR. Pre-existing CHF and PAD are independent predictors of graft loss. This warrants careful selection of transplant candidates with certain comorbidities for which a vigilant follow-up is crucial.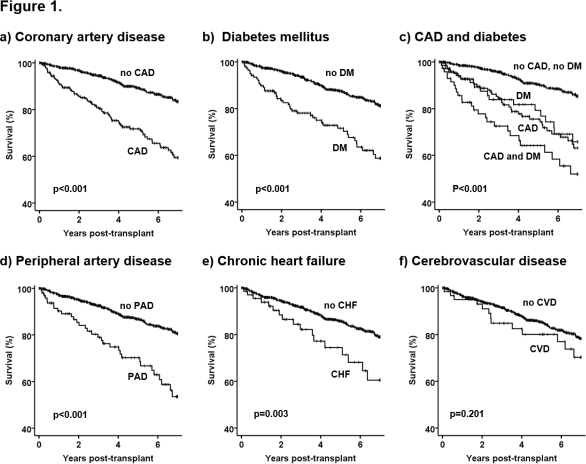
CITATION INFORMATION: Halleck F, Khadzhynov D, Lehner L, Schrezenmeier E, Duerr M, Kleinsteuber A, Budde K, Staeck O. Impact of Pre-Existing Comorbidities on Long-Term Patient and Graft Survival in Kidney Transplant Recipients. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Halleck F, Khadzhynov D, Lehner L, Schrezenmeier E, Duerr M, Kleinsteuber A, Budde K, Staeck O. Impact of Pre-Existing Comorbidities on Long-Term Patient and Graft Survival in Kidney Transplant Recipients. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-pre-existing-comorbidities-on-long-term-patient-and-graft-survival-in-kidney-transplant-recipients/. Accessed March 3, 2026.« Back to 2016 American Transplant Congress
