Impact of Pre-Donation eGFR on Long-Term Post-Donation eGFR in Younger Living Kidney Donors.
U of MN, Mpls, MN
Meeting: 2017 American Transplant Congress
Abstract number: A229
Keywords: Donation, Glomerular filtration rate (GFR), Kidney, Renal function
Session Information
Session Name: Poster Session A: Living Donor Kidney Transplant I
Session Type: Poster Session
Date: Saturday, April 29, 2017
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall D1
Objective: Most transplant centers require living kidney donors (LKDs) to have a minimum estimated glomerular filtration rate (eGFR) to ensure adequate kidney reserve to withstand age-related decline. Although some centers have lower eGFR cutoffs for older LKDs, it is unclear whether centers should have a higher eGFR threshold for younger LKDs given their longer anticipated lifespan.
Methods: We studied the longitudinal eGFR trajectory of 798 LKDs, less than 35 years of age, donating between 1980 and 2014 at a single center. The acceptance criteria used during this time included a minimum pre-donation eGFR of 80 mL/min/1.73 m2. Linear mixed-effects models, adjusting for gender, age, pre-donation BMI, smoking history, year of donation, family history of ESRD and pre-donation eGFR, were used to model eGFR after 6 weeks post-donation. We allowed pre-donation eGFR to interact with time since donation in the model to assess whether differences in pre-donation eGFR lead to long-term differences in post-doantion eGFR.
Results: Median pre-donation eGFR in this cohort was 100.0 mL/min/1.73 m2 (IQR: 89.1 – 114.1). For these younger LKDs, average kidney function increased initially during follow-up, but the rate of change depended on the pre-donation eGFR (p = 0.005; Figure 1). Holding other factors constant, a 10 mL/min/1.73 m2 increase in pre-donation eGFR was associated with a 4.96 mL/min/1.73 m2 (95% CI: 4.29 – 5.64) increase on average in eGFR 6 weeks after donation. However, by 20 and 30 years post-donation, the average difference in eGFR between LKDs with a 10 mL/min/1.73 m2 difference in pre-donation eGFR was attenuated to 3.52 mL/min/1.73 m2 (2.56 – 4.47) and 3.03 mL/min/1.73 m2 (1.93 – 4.13), respectively.
Conclusion: Differences in pre-donation kidney function are associated with only modest differences in average long-term (> 20 years) eGFR when age-related decline in this younger cohort is likely to begin. These results do not suggest that a higher eGFR cutoff should be used for younger potential LKDs.
Figure 1: Estimated average eGFR post-donation trajectory by pre-donation eGFR. All other factors held constant (25 years old, female, nonsmoker, BMI 25 kg/m2, donation year 1985, family history of ESRD). 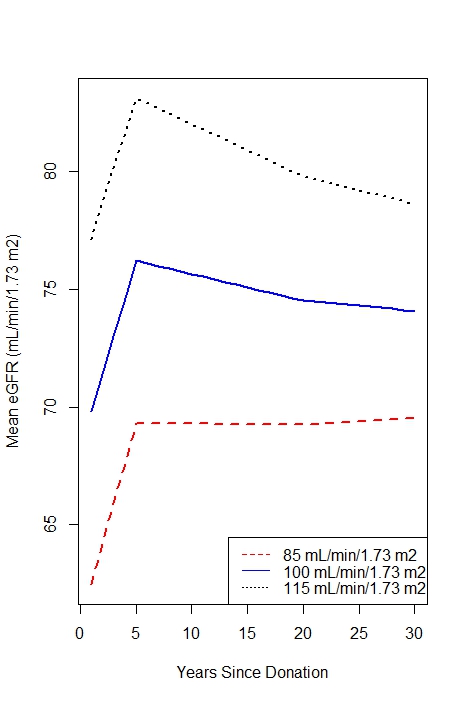
CITATION INFORMATION: Vock D, Ibrahim H, Matas A. Impact of Pre-Donation eGFR on Long-Term Post-Donation eGFR in Younger Living Kidney Donors. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Vock D, Ibrahim H, Matas A. Impact of Pre-Donation eGFR on Long-Term Post-Donation eGFR in Younger Living Kidney Donors. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-pre-donation-egfr-on-long-term-post-donation-egfr-in-younger-living-kidney-donors/. Accessed March 2, 2026.« Back to 2017 American Transplant Congress
