Identifying Health System-Level Barriers to Living Donor Kidney Transplantation: A Cross-Sectional Survey of Health Professionals
S. Sandal1, I. Schiller1, N. Dendukuri1, J. Robert1, K. Katergi1, A. Alam1, M. Cantarovich1, J. F. Fiore Jr1, C. Weber1, M. Fortin2
1McGill University, Montreal, QC, Canada, 2University of Montreal, Montreal, QC, Canada
Meeting: 2022 American Transplant Congress
Abstract number: 1733
Keywords: Living donor, Organ Selection/Allocation, Psychosocial, Public policy
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: There is growing recognition that efforts to increase living donor kidney transplantation (LDKT) should focus on health system-level inefficiencies. While previous studies focused on the perspective of patients, health professionals (HPs) may provide relevant insights into health system-level barriers to delivering LDKT. We aimed to quantify system-level barriers that HPs have identified in our previous qualitative work and compare them by LDKT performance.
*Methods: We conducted a cross-sectional survey of HPs across different transplant jurisdictions with variable LDKT performance. Participants were asked to rate several statements on a Likert scale and rate priorities to increase LDKT. Levels of agreement were assessed according to jurisdiction LDKT performance and HP characteristics.
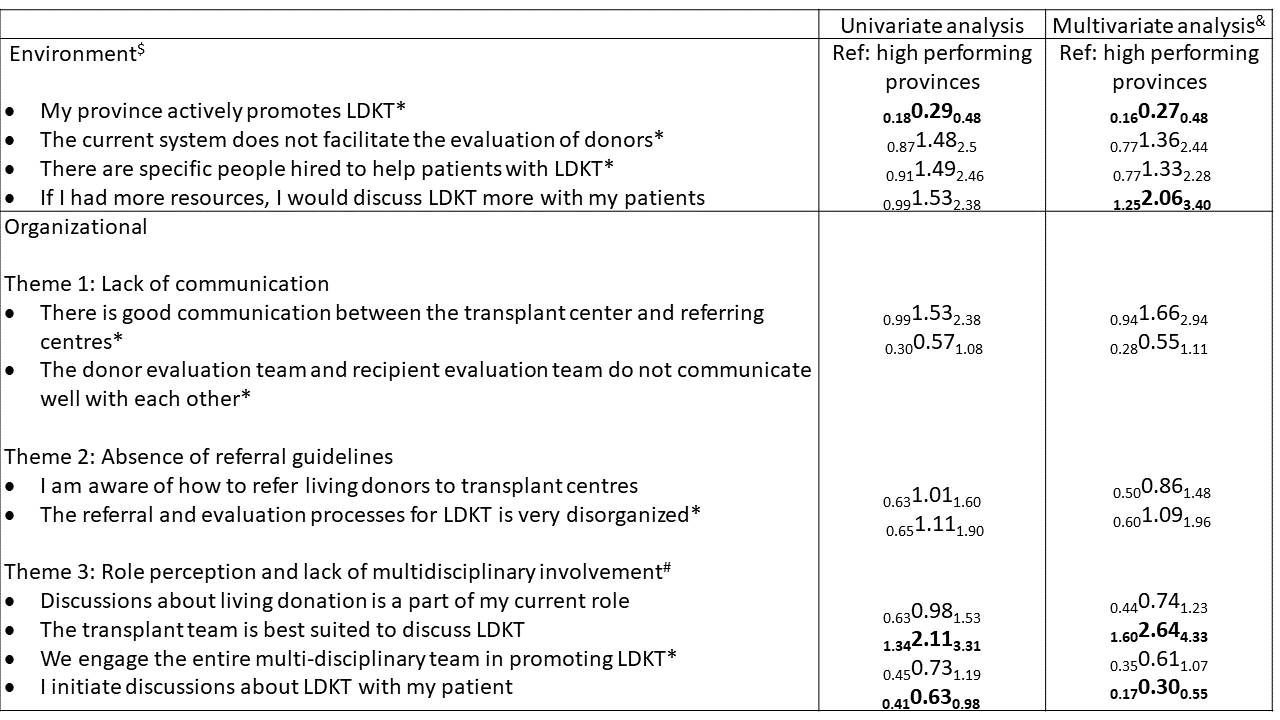
*Results: We obtained 353 complete responses. When compared with HPs from higher LDKT performing jurisdictions, HPs from lower-performing jurisdictions had lower odds of agreeing that their jurisdiction actively promoted LDKT (aOR=0.27, 95%CI:0.16-0.48) and higher odds of agreeing that if they had more resources, they would discuss LDKT more with patients (aOR=2.06, 95%CI:1.25-3.40) (Table 1). The theme of poor role perception also emerged as a notable finding. HP from lower-performing jurisdictions had lower odds of initiating discussions about LDKT with their patients (aOR=0.30, 95%CI:0.17-0.55) and higher odds of agreeing that the transplant team is best suited to discuss LDKT (aOR=2.64, 95%CI:1.60-4.33). Also, non-physicians experienced significantly more barriers across several domains. HPs ranked the following three as top priorities to increase LDKT: 1) create standardized referral and evaluation guidelines; 2) organize and streamline evaluation; and 3) provide more education and training to HPs.
*Conclusions: We report that barriers related to resources, LDKT promotion, and role perception were more prominent in lower-performing jurisdictions. HPs identified improving system-level inefficiencies and educating and training HPs as priorities to increasing LDKT. Our findings have practice and policy implications and can inform system-level interventions to improve LDKT.
To cite this abstract in AMA style:
Sandal S, Schiller I, Dendukuri N, Robert J, Katergi K, Alam A, Cantarovich M, Jr JFFiore, Weber C, Fortin M. Identifying Health System-Level Barriers to Living Donor Kidney Transplantation: A Cross-Sectional Survey of Health Professionals [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/identifying-health-system-level-barriers-to-living-donor-kidney-transplantation-a-cross-sectional-survey-of-health-professionals/. Accessed February 20, 2026.« Back to 2022 American Transplant Congress