Identification of the dnDSA Inducing HLA Mismatches Across Multiple Renal Transplant Centers: A 3-Year Longitudinal Analysis of >11,000 HLA Mismatches in 2271 Patients
1Terasaki Research Institute, Los Angeles, CA, 2Mayo Clinic, Rochester, MN, 3Mayo Clinic, Phoenix, AZ, 4East Carolina University, Greenville, NC, 5Henry Ford Transplant Institute, Detroit, MI
Meeting: 2020 American Transplant Congress
Abstract number: 205
Keywords: Antibodies, HLA antigens, HLA matching
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: The presence of a mismatch (MM) between donor and recipient HLA does not always lead to the patient developing a de novo donor-specific anti-HLA antibodies (dnDSA). A selected group of HLA MM may be more problematic when it comes to dnDSA production. The purpose of this analysis was to investigate the 3-year cumulative event rates of dnDSA development for each mismatched HLA in a large cohort of patients across four US transplant (txp) centers.
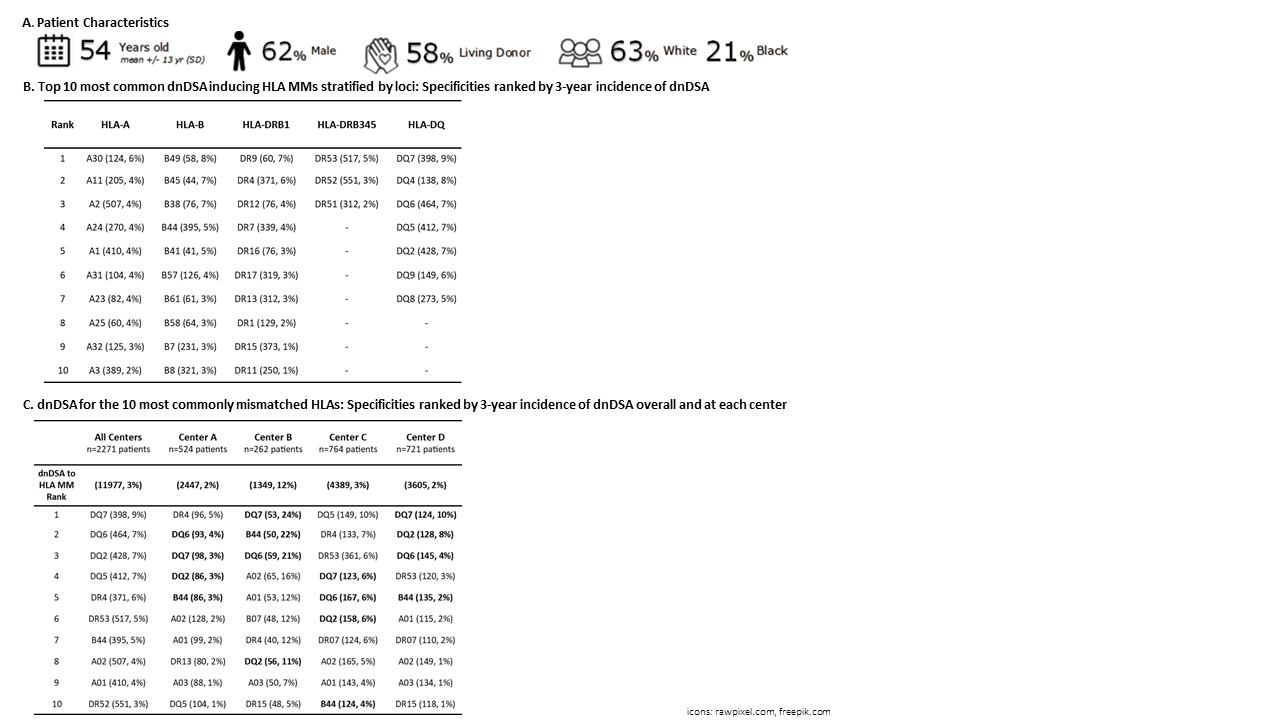
*Methods: A diverse cohort of 2271 renal txp patients with a HLA MM and without DSA at txp were analyzed (Figure A). Center-reported DSA specificity data and MFIs>999 were used to define dnDSA cases for each individual A, B, DR1, DR345, and DQ HLA MM. We assessed 3-year cumulative incidence of dnDSA by HLA specificity for each center and all centers combined. MM were excluded if they were rare (<40 MM cases across the cohort).
*Results: Within the cohort, there were 11977 HLA MMs accounting for 60 unique HLAs specificities. dnDSA developed in 7.5% (center range 3.3-24%) of patients. Of all HLA MM with at least 40 MM, the DQ7 MM induced the highest 3-year incidence of dnDSA across the cohort (Table B). Looking at the top 10 MM antigens across centers, the specificities were nearly identical but the 3-year dnDSA post-txp incidence at these specificities differed (Table C). dnDSA to DQ7, DQ6, B44, and DQ2 appeared at the top of each center’s list but the incidence was higher at some centers.
*Conclusions: This study suggests that HLA dnDSA rates by MM differs between centers but the most problematic ones such as DQ7, DQ6, and DQ2 remain the same across centers. Additionally, among common HLA mismatches that are difficult to avoid, dnDSA rate differences give insight into a more advanced allocation scheme aiming to prevent dnDSA.
To cite this abstract in AMA style:
Brennan JM, Stegall MD, Schinstock CA, Heilman RL, Rebellato LM, Samaniego-Picota MD, Lesser D, Ghandi MJ, Beaumont JL, Everly MJ. Identification of the dnDSA Inducing HLA Mismatches Across Multiple Renal Transplant Centers: A 3-Year Longitudinal Analysis of >11,000 HLA Mismatches in 2271 Patients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/identification-of-the-dndsa-inducing-hla-mismatches-across-multiple-renal-transplant-centers-a-3-year-longitudinal-analysis-of-11000-hla-mismatches-in-2271-patients/. Accessed February 25, 2026.« Back to 2020 American Transplant Congress