Hyperammonemia Syndrome in a Kidney Transplant Recipient Caused by Quinolone-Resistant Ureaplasma Infection
A. B. Higgins1, R. Rogers2, A. J. Osband3, R. Gohh4, P. Morrissey3, A. Seo1, B. Chen1, D. Crabb5, S. Leal5, K. Waites5, D. Farmakiotis2, G. J. Nau2
1Department of Medicine, Alpert Medical School of Brown University, Providence, RI, 2Division of Infectious Diseases, Alpert Medical School of Brown University, Providence, RI, 3Department of Surgery, Alpert Medical School of Brown University, Providence, RI, 4Division of Nephrology, Alpert Medical School of Brown University, Providence, RI, 5Division of Laboratory Medicine, Department of Pathology, University of Alabama at Birmingham, Birmingham, AL
Meeting: 2020 American Transplant Congress
Abstract number: A-198
Keywords: Bacterial infection, Hypogammaglobulinemia, Infection, Kidney/liver transplantation
Session Information
Session Name: Poster Session A: Kidney Infectious Excluding Polyoma & Viral Hepatitis
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Urease-producing bacteria release significant amounts of ammonia. Donor-derived Ureaplasma infections in lung transplant recipients have been implicated in the pathogenesis of hyperammonemia syndrome (HS). In such cases, clinicians often opt for long courses of ≥2 antibiotics, but antimicrobial resistance (R) is rarely documented and its frequency is unknown.
*Methods: We present the first, to our knowledge, case of HS caused by levofloxacin (lvq)-R U. urealyticum infection in a kidney transplant (KT) recipient.
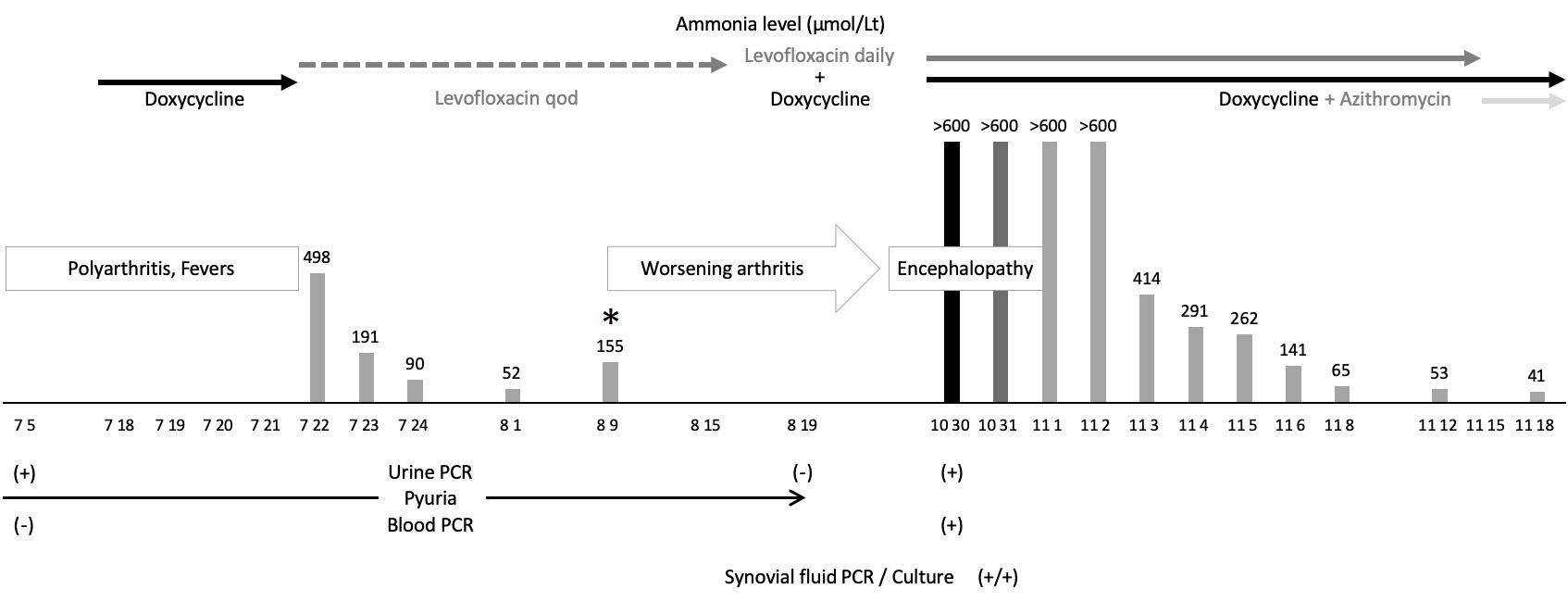
*Results: A 16-year-old female with end-stage renal disease from systemic lupus erythematosus underwent deceased donor KT. For 10 months, serum creatinine (Cr) was <1 mg/dL. She then developed sterile pyuria and renal dysfunction (Cr 1.6-4.4). Two renal biopsies showed interstitial inflammation, one also granulomas. Infectious disease work-up, including next-generation DNA sequencing of allograft tissue for bacterial pathogens, was unrevealing. When she developed polyarthritis and fever, blood and urine Ureaplasma-Mycoplasma PCR were sent. Urine PCR was positive for U. urealyticum. After 3 days of doxycycline (doxy), ammonia level was checked and was 498 (normal <50) µmol/L, despite no encephalopathy. Renally-dosed lvq (q.o.d.) was administered for 3 weeks with resolution of pyuria and negative repeat urine PCR. Ammonia levels initially decreased, but increased again while on lvq (Fig. 1: *). Two months later, she was admitted with worse polyarthritis, confusion, asterixis and ammonia >600. Blood PCR, urine PCR, left knee synovial fluid PCR and culture were now positive. She was started on daily lvq+doxy. Ammonia levels normalized and all symptoms improved. Susceptibility testing (ST) showed lvq-R (MIC 32 mg/L), therefore lvq was changed to azithromycin, with ongoing clinical improvement.
*Conclusions: The frequency of Ureaplasma infections is likely underestimated. ST should be performed in Ureaplasma strains isolated from extragenital specimens. In transplant recipients with HS, empiric treatment with ≥2 antibiotics may be indicated.
To cite this abstract in AMA style:
Higgins AB, Rogers R, Osband AJ, Gohh R, Morrissey P, Seo A, Chen B, Crabb D, Leal S, Waites K, Farmakiotis D, Nau GJ. Hyperammonemia Syndrome in a Kidney Transplant Recipient Caused by Quinolone-Resistant Ureaplasma Infection [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/hyperammonemia-syndrome-in-a-kidney-transplant-recipient-caused-by-quinolone-resistant-ureaplasma-infection/. Accessed March 5, 2026.« Back to 2020 American Transplant Congress