Hospitalization, Dialysis Center Type, and Disparities in ESRD Survival and Waitlist Access
Surgery, Emory University, Atlanta, GA.
Meeting: 2018 American Transplant Congress
Abstract number: A305
Keywords: Economics, Kidney transplantation, Resource utilization, Survival
Session Information
Session Name: Poster Session A: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: Excess hospitalization has been shown to reduce kidney transplant waitlist survival and likelihood of transplant. We studied hospitalization as a predictor of waitlist access in the context of known sociodemographic disparities.
Methods: United States Renal Data Systems records from 2002-2015 were used to identify all incident adult cases of end stage renal disease (ESRD) with continuous Medicare coverage for the first year following ESRD onset. Patients were categorized by race, comorbidities, and sociodemographic predictors including county community health score (CHS) and poverty, as well as characteristics of first dialysis center and days spent inpatient in the 12 months following ESRD onset. Cox multivariable analysis was used to examine the relationship between these risk factors and waitlisting and 5 year survival.
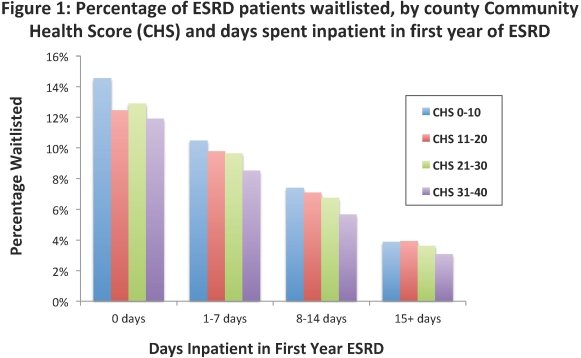
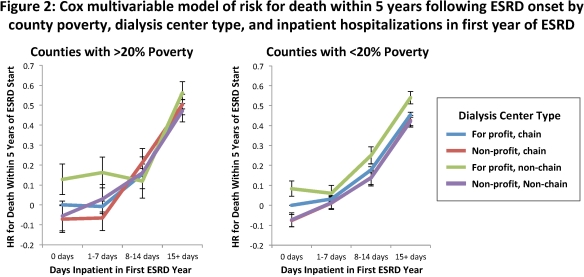
Results: Among 348,817 patients, the overall waitlisting rate was 8.4%. Frequent hospitalization and sociodemographic disadvantage were associated with decreased survival and waitlist access (Figure 1). Admissions were more frequent among poor than affluent communities (37% vs. 32% admitted > 14 days for CHS 31-40 vs. CHS 0-10 counties, p < 0.001), but impact of successive hospitalization on access and survival was stable across CHS levels. Poor communities were more reliant on for-profit dialysis centers. In multivariable analysis, impact of dialysis center type on survival differed by community poverty level, with for-profit, non-chain centers tending toward inferior outcomes at all levels of admission intensity (Figure 2).
Conclusions: Baseline admissions early after ESRD onset predict subsequent survival and likelihood of waitlisting across sociodemographic strata. Higher rates of hospitalization for patients in disadvantaged communities and dialyzing at for-profit centers may explain decreased waitlist access and survival rates.
CITATION INFORMATION: Lynch R., Zhang R., Adams A., Patzer R. Hospitalization, Dialysis Center Type, and Disparities in ESRD Survival and Waitlist Access Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Lynch R, Zhang R, Adams A, Patzer R. Hospitalization, Dialysis Center Type, and Disparities in ESRD Survival and Waitlist Access [abstract]. https://atcmeetingabstracts.com/abstract/hospitalization-dialysis-center-type-and-disparities-in-esrd-survival-and-waitlist-access/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress