HLA-DR/DQ Single Molecule Eplet Mismatch and Formation of De Novo Donor-Specific Anti-HLA Antibodies After Kidney Transplantation in Children
1Division of Nephrology, Department of Pediatrics, Stanford University, Palo Alto, CA, 2Histocompatibility and Immunogenetics Laboratory, Stanford Blood Center, Palo Alto, CA
Meeting: 2022 American Transplant Congress
Abstract number: 107
Keywords: Antibodies, Immunosuppression, Rejection
Topic: Clinical Science » Kidney » 43 - Kidney: Pediatrics
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:00pm-6:10pm
Presentation Time: 6:00pm-6:10pm
Location: Hynes Ballroom C
*Purpose: The advances in HLA typing methods and elucidation of three-dimensional molecular structures of HLA antigens in recent years have allowed analysis of donor/recipient HLA mismatches at the structural level, which may be a more precise and optimal approach to determine HLA compatibility and predict transplant outcomes. Eplet mismatches in HLA, especially HLA-DR/DQ at the single-molecule level, have been identified as a prognostic biomarker for primary alloimmunity. There have been limited studies evaluating this approach and the optimal risk stratification cut-offs in racially diverse pediatric patients receiving kidney transplantation.
*Methods: Children who underwent kidney transplantation from 1/1/2010-3/1/2018 at Stanford, with at least 12-month follow-up, were included. High-resolution HLA typing was performed using next generation sequencing. HLA Matchmaker software (HLA DRDQDP Matching version 2.0) was used to count eplet mismatches for donor/recipient pairs. Outcome of interest was time to de novo donor specific antibody (dnDSA) formation. dnDSA were screened at the time of transplant, 1, 2, 3, 6, and 12 months following, at least annually thereafter, and as clinically indicated. ROC analysis at the DR and DQ loci was performed to determine risk categories based on total and single-molecule eplet mismatch thresholds. Survival analysis was performed by the Kaplan-Meier method using the log-rank test for significance.
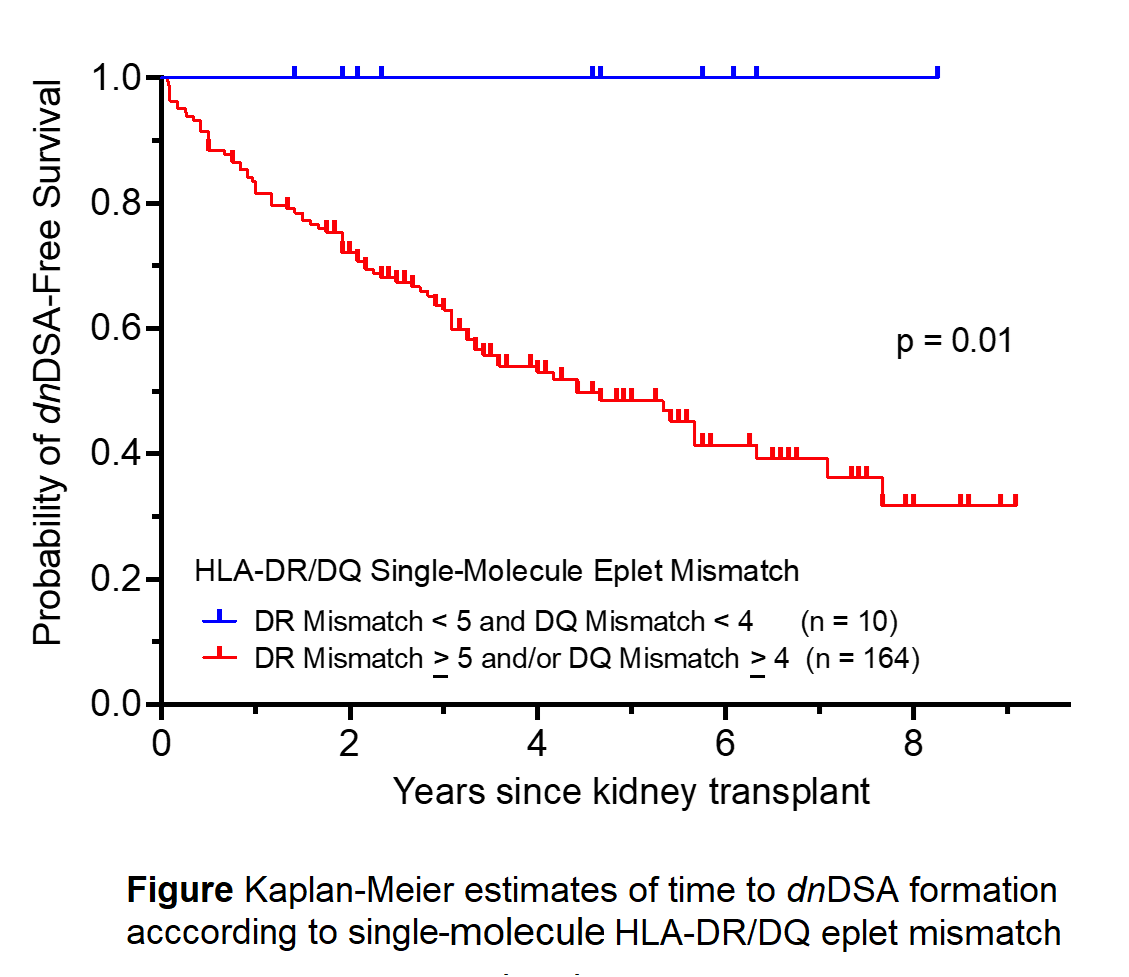
*Results: A total of 233 patients were identified. Our preliminary results include high‑resolution typing for 174. Of those, median age was 13 (IQR 9), 23.6% had living donor transplant and 48.3% were female. The Median follow-up time was 36.5 months (IQR 36). 46.0% formed Anti-HLA class II dnDSA. Patients with an eplet mismatch sum of HLA DR > 6 and/or DQ > 4 (n=161) had increased risk of HLA-DR/DQ dnDSA formation, p=0.006. Similarly, patients with single-molecule HLA-DR > 5 and/or DQ > 4 had an increased risk of HLA-DR/DQ dnDSA development. [Figure]
*Conclusions: Single-molecule eplet mismatch and total eplet mismatch are associated with an increased risk of dnDSA formation. Assessing a patient’s individual risk based on donor/recipient HLA-DR/DQ eplet mismatches may guide immunosuppression regimen in the post-transplant period and predict adverse outcomes.
To cite this abstract in AMA style:
Sigurjonsdottir VK, Piburn K, Grimm PC, Zhang BM. HLA-DR/DQ Single Molecule Eplet Mismatch and Formation of De Novo Donor-Specific Anti-HLA Antibodies After Kidney Transplantation in Children [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/hla-dr-dq-single-molecule-eplet-mismatch-and-formation-of-de-novo-donor-specific-anti-hla-antibodies-after-kidney-transplantation-in-children/. Accessed February 18, 2026.« Back to 2022 American Transplant Congress