Heart Transplantation Outcomes in Multiorgan Transplants
1LAC+USC, Los Angeles, CA, 2The Queens Medical Center, Honolulu, HI, 3UCLA Medical Center, Los Angeles, CA, 4University of Arizona Sarver Heart Center, Tucson, AZ, 5Harbor-UCLA Medical Center, Los Angeles, CA, 6Newark Beth-Israel, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: B-270
Keywords: Allocation
Session Information
Session Name: Poster Session B: Heart and VADs: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: We sought to elucidate the differences in outcomes between patients undergoing Heart-Lung (HL) Heart-Lung-Kidney (HLK) and Heart-Lung-Liver (HLL) multiorgan transplantation.
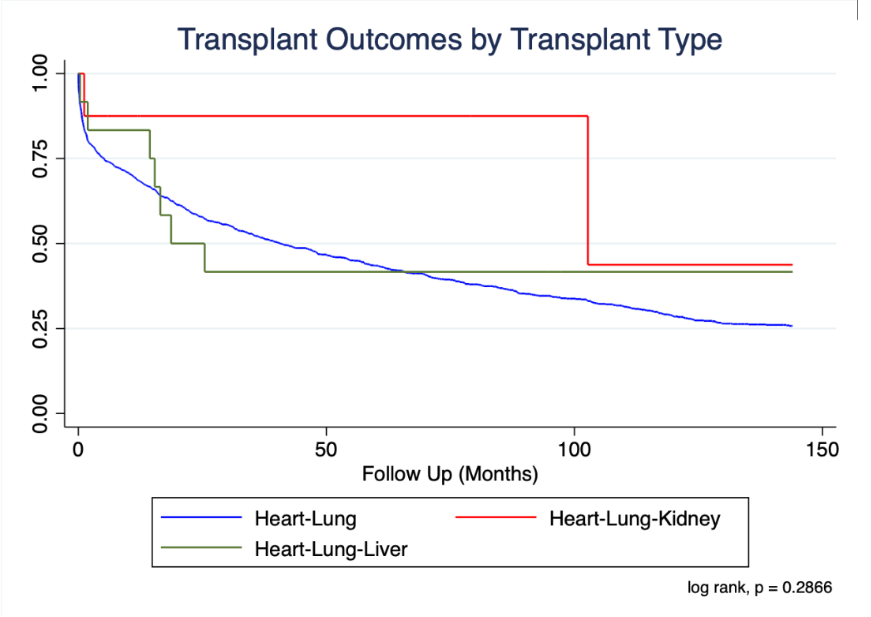
*Methods: Using the UNOS registry, we compared outcomes in HL, HLK, and HLL recipients. Analysis was performed using multivariate Cox proportional hazard regression model that adjusted for age, sex, race, diagnosis of diabetes, ischemic time, recipient wait-time, HLA mismatch, need for dialysis, and need for life support. We excluded patients who were age less than 18 years old or who were lost-to-follow-up. Kaplan-Meier survival analysis was performed.
*Results: 1177 HL patients, 8 HLK, and 12 HLL patients were identified. There was no significant difference in mortality between the three groups. HL recipients were more likely to have undergone prior non-transplant cardiac surgery (HL 91.6% vs HLK 75.0% vs HLL 75.0% p=0.033). HLK patients were more likely to require VAD support (HL 1.2% vs HLK 12.5% vs HLT 0.0% p=0.015), have higher serum creatinine (HL 1.0 mg/dL ± 0.6 vs HLK 2.4 ± 1.3 vs HLL 0.9 ± 0.5 p<0.001), require dialysis (HL 1.5% HLK 37.5% and HLL 0.0% p<0.001), and have higher pulmonary capillary wedge pressures (HL 15.5mmHg ± 9.4 vs HLK 26.2 ± 11.0 vs HLL 13.0 ± 10.1 p=0.038).
*Conclusions: Despite increasing risk factors, HL concomitant with either kidney or liver transplant did not affect survival compared to HL alone. Carefully selected patients may benefit from triple organ transplantation, however, ethical issues of organ utilization may arise.
To cite this abstract in AMA style:
Kingsford P, Li JP, Lum CJ, Salimbangon A, Liu G, Wolfson AM, Chand RR, Banankhah P, Genyk PA, Vucicevic D, Pandya K, Rahman J, Fong M, Grazette L, Kiankhooy A, Nattiv J, Hashmi S, Nuno SB, Pizula J, Miklin DJ, Lee AE, Yang K, Shah S, Vaidya AS, DePasquale EC. Heart Transplantation Outcomes in Multiorgan Transplants [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/heart-transplantation-outcomes-in-multiorgan-transplants/. Accessed February 24, 2026.« Back to 2020 American Transplant Congress