Greater Susceptibility for Metabolic Syndrome in Pediatric Transplant Recipients – A Case-Control Study
R. Bloete,1 N. Memaran,1 B. Borchert-Mörlins,1 D. Thurn,1 E. Bauer,1 R. Büscher,2 J. Oh,3 B. Schmidt,4 A. Melk.1
1Department of Pediatric Kidney, Liver and Metabolic Diseases, Hannover Medical School, Hanover, Germany
2Department of Pediatric Nephrology, University Hospital Essen, Essen, Germany
3Department of Pediatric Nephrology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
4Department of Nephrology, Hannover Medical School, Hanover, Germany.
Meeting: 2018 American Transplant Congress
Abstract number: B214
Keywords: Immunosuppression, Metabolic complications, Obesity, Post-transplant hypertension
Session Information
Session Name: Poster Session B: Kidney: Pediatrics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Introduction. Metabolic syndrome not only contributes to an increased risk for cardiovascular sequelae but is also associated with impaired graft function and lower graft survival after adult renal transplantation, however, prevalence in pediatric transplant recipients is not sufficiently investigated.
Methods. In a prospective, multicenter case-control study, we assessed the disposition towards post-transplant metabolic syndrome (PTMS) in 295 pediatric transplant recipients compared to 1.475 age and gender matched healthy controls from the German Health Survey for Children and Adolescents (KiGGS). PTMS was defined as the co-occurrence of any three of the five conditions: obesity, hypertension, hypertriglyceridemia, reduced high-density lipoprotein and diabetes mellitus.
Results. PTMS was more common after pediatric kidney (KTx), lung (LuTx), liver (LTx), or stem cell transplantation (ScTx) compared to non-transplanted peers (p≤0.007): 39% of patients after KTx (Odds ratio (OR) 16.2; 95%Confidence interval (CI) 9.1-28.9), 43% after LuTx (OR 21.8; 95%CI 8.2-57.4), 16% after LTx (OR 4.6; 95%CI 2.1-10.1), 13% following ScTx (OR 3.7; 95% CI 1.4-9.5) were affected compared to 4% of the controls.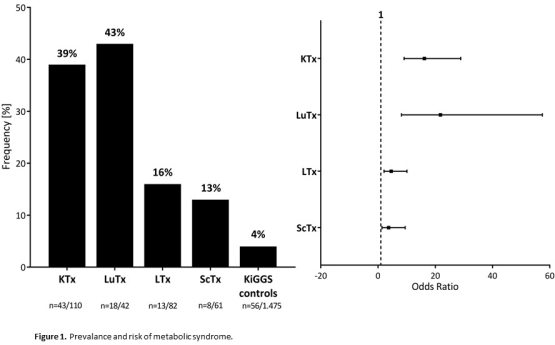 KTx (OR 3.1) and ScTx (OR 3.7) patients were more likely to be obese (p<0.001). Older age, less physical activity, type of immunosuppression, and hypovitaminosis D contributed to the risk for PTMS.
KTx (OR 3.1) and ScTx (OR 3.7) patients were more likely to be obese (p<0.001). Older age, less physical activity, type of immunosuppression, and hypovitaminosis D contributed to the risk for PTMS.
Conclusion. In conclusion, PTMS is highly prevalent among pediatric transplant recipients with KTx and LuTx patients constituting a high-risk group. Early diagnosis and tailored treatment of the modifiable components is important to lower patients' cardiovascular risk.
CITATION INFORMATION: Bloete R., Memaran N., Borchert-Mörlins B., Thurn D., Bauer E., Büscher R., Oh J., Schmidt B., Melk A. Greater Susceptibility for Metabolic Syndrome in Pediatric Transplant Recipients – A Case-Control Study Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bloete R, Memaran N, Borchert-Mörlins B, Thurn D, Bauer E, Büscher R, Oh J, Schmidt B, Melk A. Greater Susceptibility for Metabolic Syndrome in Pediatric Transplant Recipients – A Case-Control Study [abstract]. https://atcmeetingabstracts.com/abstract/greater-susceptibility-for-metabolic-syndrome-in-pediatric-transplant-recipients-a-case-control-study/. Accessed February 16, 2026.« Back to 2018 American Transplant Congress
