Four Separate Frailty Metrics Lack Concordance and Are Non-Reflective of the Kidney Transplant Listing Outcome: A Large Single Center Review
Transplant Surgery, Emory University Hospital, Atlanta, GA
Meeting: 2022 American Transplant Congress
Abstract number: 312
Keywords: Kidney, Prediction models, Waiting lists
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Name: Health Equity and Access I
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:30pm-6:40pm
Presentation Time: 6:30pm-6:40pm
Location: Hynes Ballroom C
*Purpose: It is well known that functional status has prognostic value for post-surgical outcomes, however pre-transplant patients are not required to undergo objective frailty testing. Currently used Karnofsky Performance Scores have limited ability to stratify patients. Here we studied renal failure patients referred for transplant evaluation through four different frailty metrics, comparing their concordance and differences after the listing decision.
*Methods: We investigated four metrics for frailty in patients who presented for renal transplant evaluation between 4/22/2019 and 11/15/2019. 289 patients underwent both cross-sectional imaging allowing calculation of a psoas muscle index (PMI) score, and calculation of a modified Frailty Risk Score (FRS) determined by retrospective chart review of 15 criteria. Of these patients, 183 were also evaluated using the Fried Frailty score (FFS). UNET was queried for EPTS score for post-transplant patients. Fisher tests were used to compare frailty assessments and t-tests were used to compare EPTS scores.
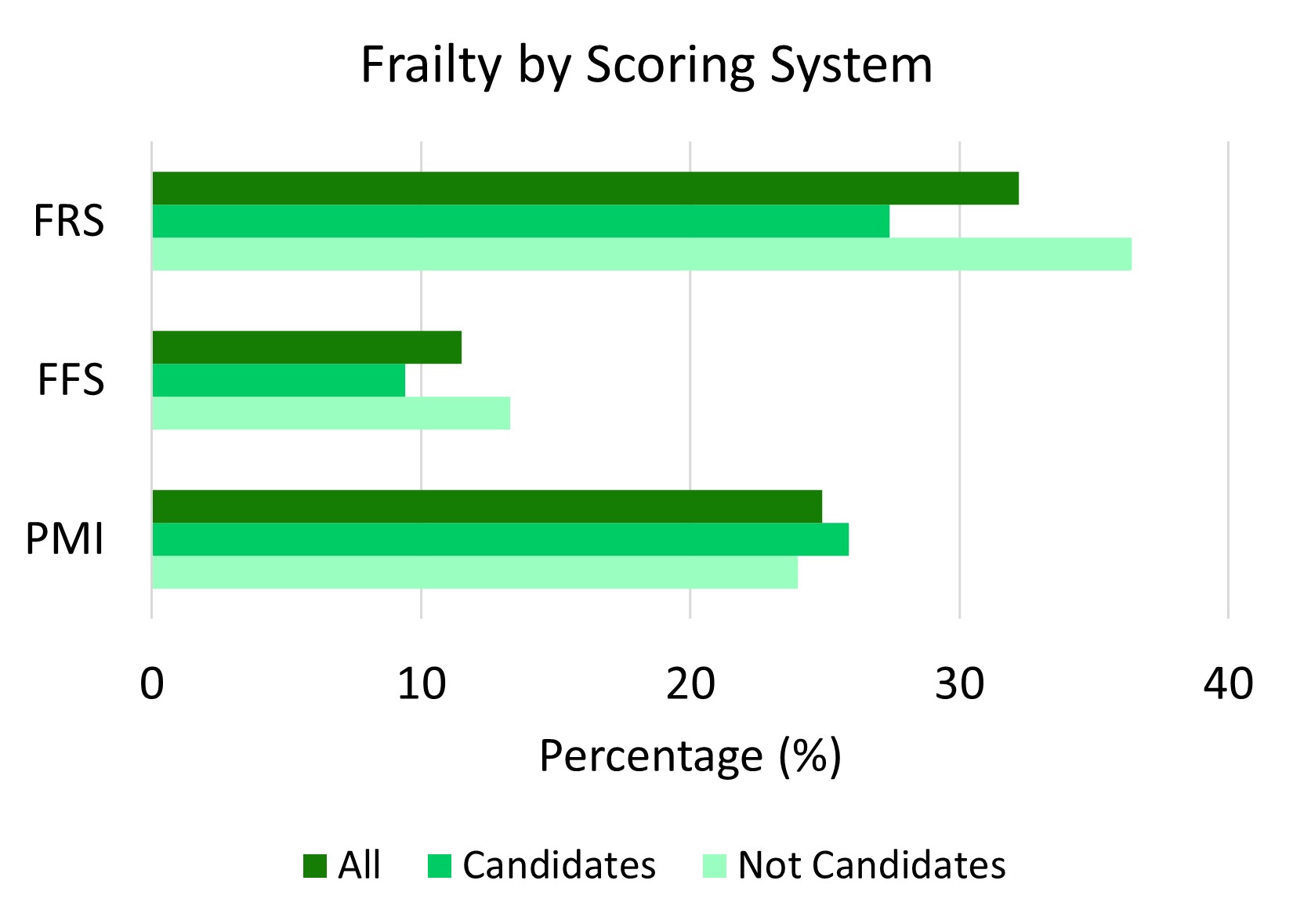
*Results: In total 151 (52.2%) patients were considered frail by at least one metric. 24.9%, 11.5%, and 32.2% of all evaluated patients were considered frail based on PMI, FFS and FRS, respectively, and of the listed candidates 25.9%, 9.4%, and 27.4% were frail by PMI, FFS and FRS, respectively. There was no difference in the percentage of evaluated patients categorized as frail between those listed versus those deemed not a candidate for transplant. Concordance between metrics was poor with only 20.2% of the total frail patients being classified as frail by more than one score. One patient was deemed frail by all three scales. PMI and FRS were more sensitive compared to FFS for identifying frail patients (p=0.0003 and p=0.0001 respectively). Average EPTS score at time of transplant for frail patients (defined as frail on at least one score) was 49 versus 40 for non-frail patients (p=0.2646).
*Conclusions: Frailty could be defined by PMI, FFS, and FRS, but this was not consistent for individual patients. PMI and FRS were more sensitive metrics than FFS. Although not statistically significant, EPTS differences were evident across frail and non-frail patients. Ultimately the patients successfully listed for transplant did not vary in frailty metrics from those who were not listed. These findings suggest frail patients have access to transplant at our center and that concordant objective metrics which can be tracked over time are needed.
To cite this abstract in AMA style:
Cimeno A, Lewis G, Parsons R. Four Separate Frailty Metrics Lack Concordance and Are Non-Reflective of the Kidney Transplant Listing Outcome: A Large Single Center Review [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/four-separate-frailty-metrics-lack-concordance-and-are-non-reflective-of-the-kidney-transplant-listing-outcome-a-large-single-center-review/. Accessed March 4, 2026.« Back to 2022 American Transplant Congress