Factors Influencing Emergency Department Utilization and Hospital Re-Admissions in an Adult Urban Renal Transplant Population
1University of Illinois at Chicago, Chicago, IL, 2University of Chicago Medicine, Chicago, IL
Meeting: 2020 American Transplant Congress
Abstract number: B-222
Keywords: Kidney transplantation, Obesity, Resource utilization
Session Information
Session Name: Poster Session B: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Emergency department (ED) visits and hospital re-admissions increase morbidity, decrease quality of life, and increase healthcare costs after renal transplant (RT). The purpose of this study was to compare outcomes of adult RT recipients according to acute care utilization to determine risk factors for emergency department visitations and re-hospitalizations.
*Methods: Single-center retrospective cohort study of adult RT recipients between 09/2013 and 09/2016. All data was obtained via electronic medical record; diagnoses were categorized. by Patients were compared across number of ED visits and then by hospital re-admissions. Univariate and multivariate logistic regression model was constructed to assess risk factors for multiple acute care utilizations within the first year of RT.
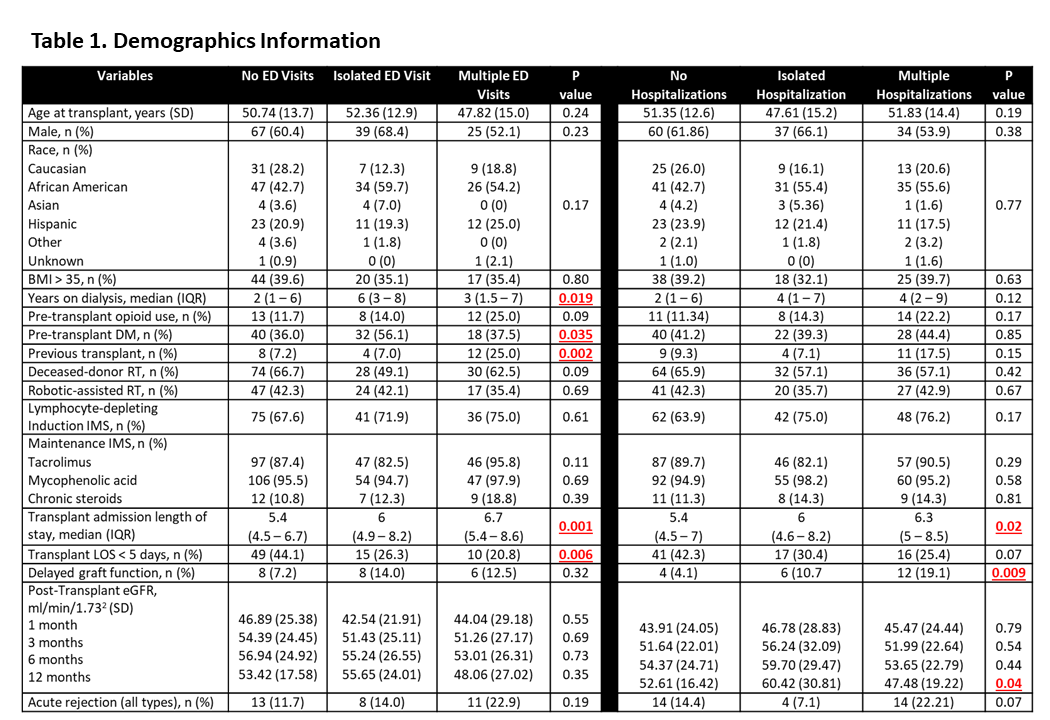
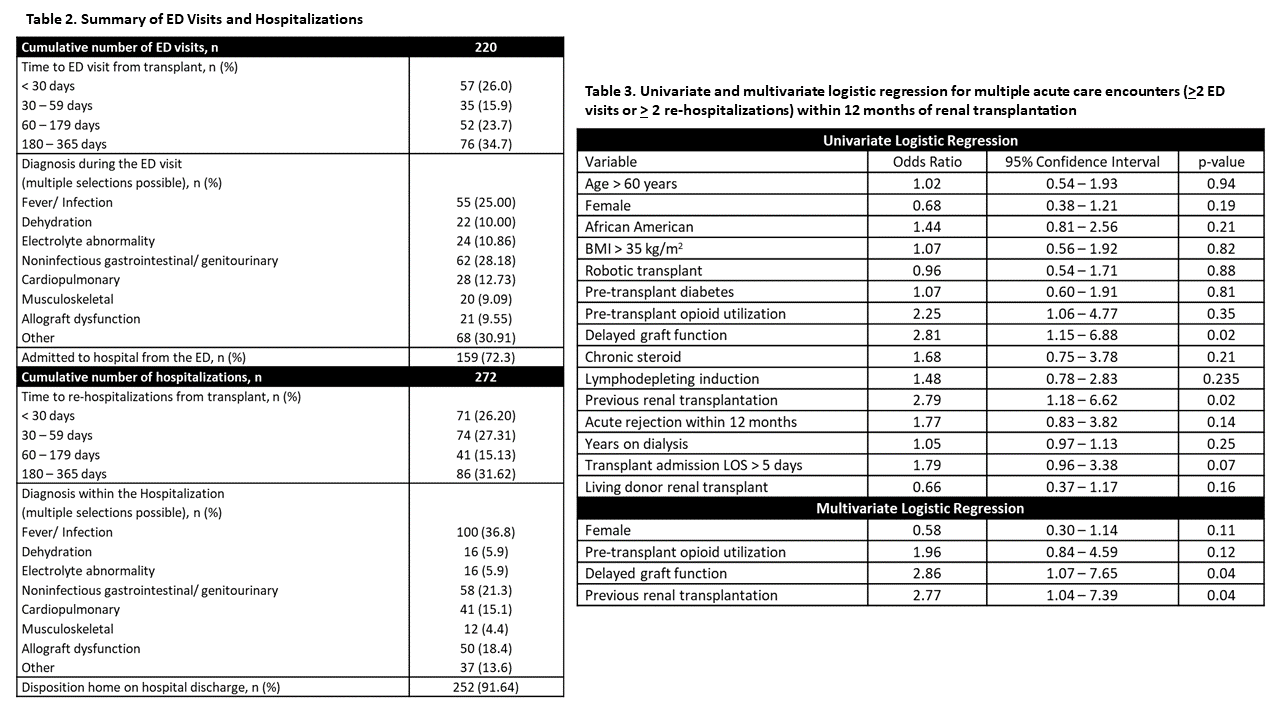
*Results: 216 patients were included. Patients were 50.5 (SD +/- 13.9) years old, predominantly African American (49.77%), with an average BMI of 33.33 (SD +/- 9.8) and received deceased donor RTs (61.11%). A total of 105 (48.6%) patients visited the ED within the first year of RT (26.4% had single ED visits and 22.2% had multiple ED visits). A total of 119 (55.1%) patients had at least one hospital re-admission within the first year of RT; 25.9% experienced an single hospital re-admission and 29.2% experienced multiple hospital re-admissions. Table 1 highlights demographic differences. Table 2 summarizes ED visits and re-hospitalizations across the cohort. Obesity did not impact ED visits or re-hospitalizations (p>0.05 for both). In multivariate logistic regression analysis, delayed graft function (OR 2.86, 95% CI 1.07 -7.65) and previous renal transplant (OR 2.77, 95% CI 1.04 -7.39) were associated with multiple acute care utilizations (Table 3).
*Conclusions: Acute care utilization following RT is high. Our findings were similar to previously reported experiences. Obesity was not associated with re-hospitalization and ED visits post-RT. Strategies addressing potential preventable ED visits and hospital re-admissions should be promoted to help improve patient care and increase efficiency of acute care resources.
To cite this abstract in AMA style:
Lichvar A, Patel A, Gimbar RPetzel, Pierce D, Tzvetanov I, Benedetti E, Campara M. Factors Influencing Emergency Department Utilization and Hospital Re-Admissions in an Adult Urban Renal Transplant Population [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/factors-influencing-emergency-department-utilization-and-hospital-re-admissions-in-an-adult-urban-renal-transplant-population/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress