Expanding the Deceased Donor Pool
Int Med, Univ of Calif Davis, Sacramento, CA
Surgery, Univ of Calif, Davis, Sacramento, CA
Meeting: 2013 American Transplant Congress
Abstract number: 302
The rate of listing of candidates for kidney transplantation continues to exceed the rate of transplantation. To narrow this gap the conventional boundaries for deceased donor (DD) kidneys have been pushed. We hypothesized the outcome for the non-conventional deceased donor (NCDD) kidney transplant would be acceptable for recipient and graft survival as compared to standard criteria donor (SCD) transplants.
Methods: Since 2005 we accepted the following DD: peds-en-bloc, expanded criteria (ECD), kidneys with acute kidney injury (AKI), donation after circulatory death kidneys (DCD), Hep C +ve, and Hep B core Ab +ve. We included all DD transplants done between Jan 2005 and July 2012 and evaluated patient survival (PS) and graft survival (GS) out to 5 yrs and e-GFR out to 3 yrs.
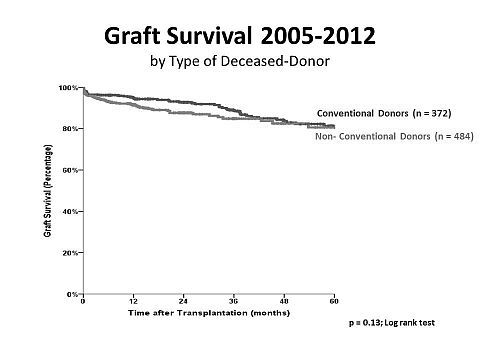
Results: 484 NCDD were done at our center between 2005 and 2012. Of these 31% were ECD, 31% DCD, 24% peds-en-bloc, 4% dual adult donors, 25% AKI, 4.5% HCV+, and 13% HepBcAb+ (some donors fit more than one category). DGF was noted in 28% of NCDD vs 13% SCD kidneys (p < 0.001). Complications < 90 days occurred in 19% of the NCDD vs 15% for SCD (p=0.1), and graft failure < 90 days were 5% for NCDD vs. 3% for SCD (p=0.1). GS was not different between groups (80.6% vs 81.3% for SCD at 5 yrs; NCDD vs SCD, respectively; p=0.13). Likewise, PS was not different between groups (89.6% for NCDD vs 90% for SCD at 5 yrs; p=0.09).
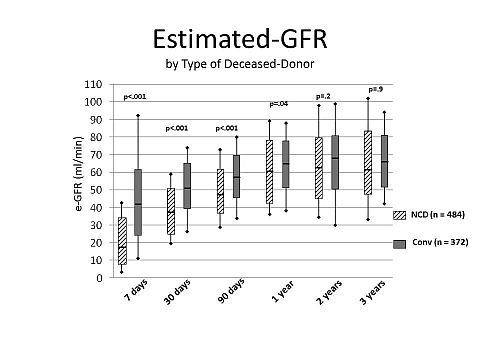
The e-GFR was lower for the NCDD recipients within the first yr (63 ± 26.6 vs. 70 ± 61.7 ml/min, NCDD vs SCD, respectively; p=0.04) but by 2 yrs there was no difference between the two (67 ± 32.2 vs. 71 ± 41.1 ml/min, NCDD vs SCD, respectively; (p=0.2).
Conclusion: Use of NCDD is associated with an increase in DGF, but no difference in short or long term patient or graft survival or kidney function. Centers should carefully consider NCDD to increase the donor pool.
To cite this abstract in AMA style:
Adey D, Perez R, Alnimri M, Mattos Ade. Expanding the Deceased Donor Pool [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/expanding-the-deceased-donor-pool/. Accessed February 6, 2026.« Back to 2013 American Transplant Congress
