Expanding A2 to B Kidney Transplantation: Safe and Effective Use of Recipients with High Titer Antibodies
1Medstar Georgetown Transplant Institute, Washington, DC, 2Department of Surgery, Johns Hopkins Medical Center, Baltimore, MD
Meeting: 2021 American Transplant Congress
Abstract number: 132
Keywords: Donors, marginal, Kidney transplantation, Outcome
Topic: Clinical Science » Kidney » Kidney Deceased Donor Selection
Session Information
Session Name: Kidney Deceased Donor Selection
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 5:00pm-5:05pm
Presentation Time: 5:00pm-5:05pm
Location: Virtual
*Purpose: Minor ABO incompatible (ABOi) transplants from blood group A2 or A2B donors have increased since 2014, but virtually all centers limit recipients to having anti-A titers of 1:4 or less. We reviewed our center’s experience transplanting patients with higher anti-A titers and their longer term outcomes.
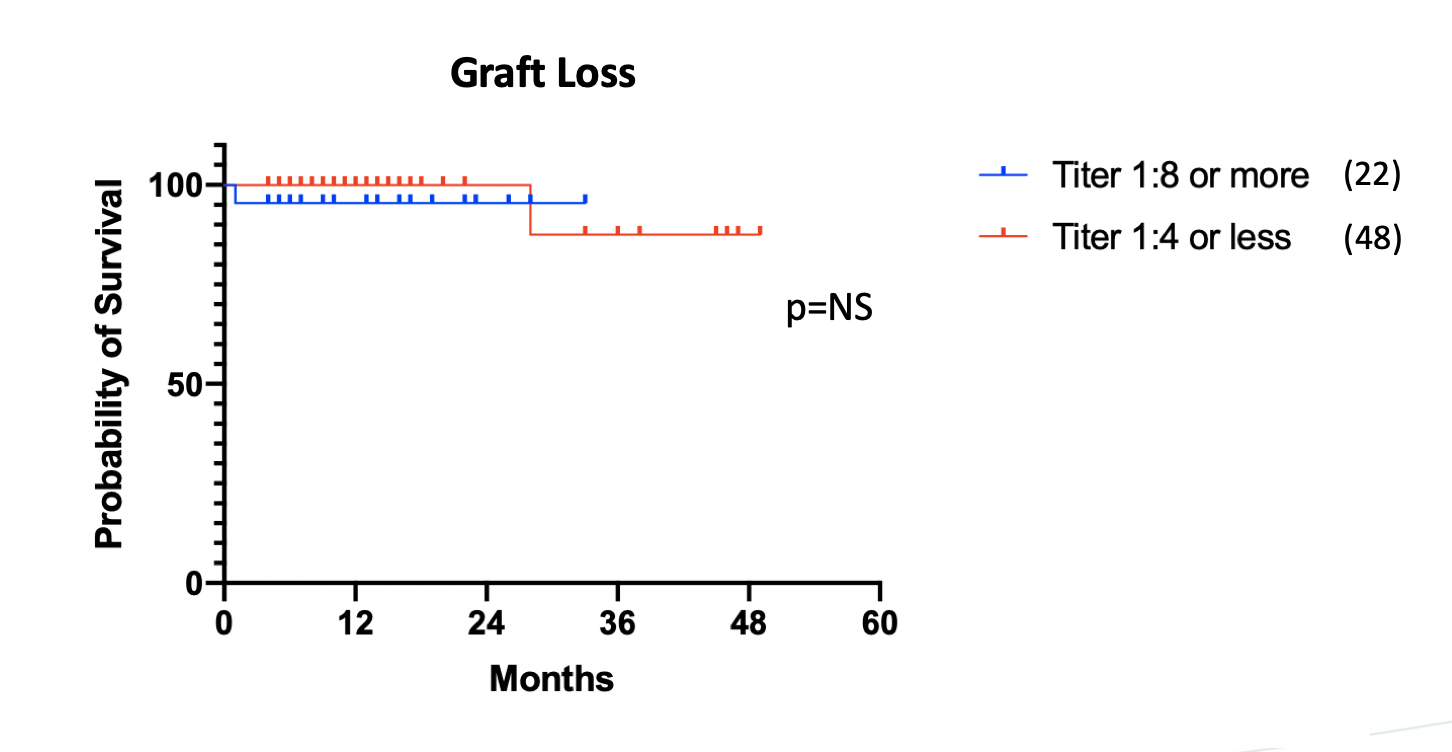
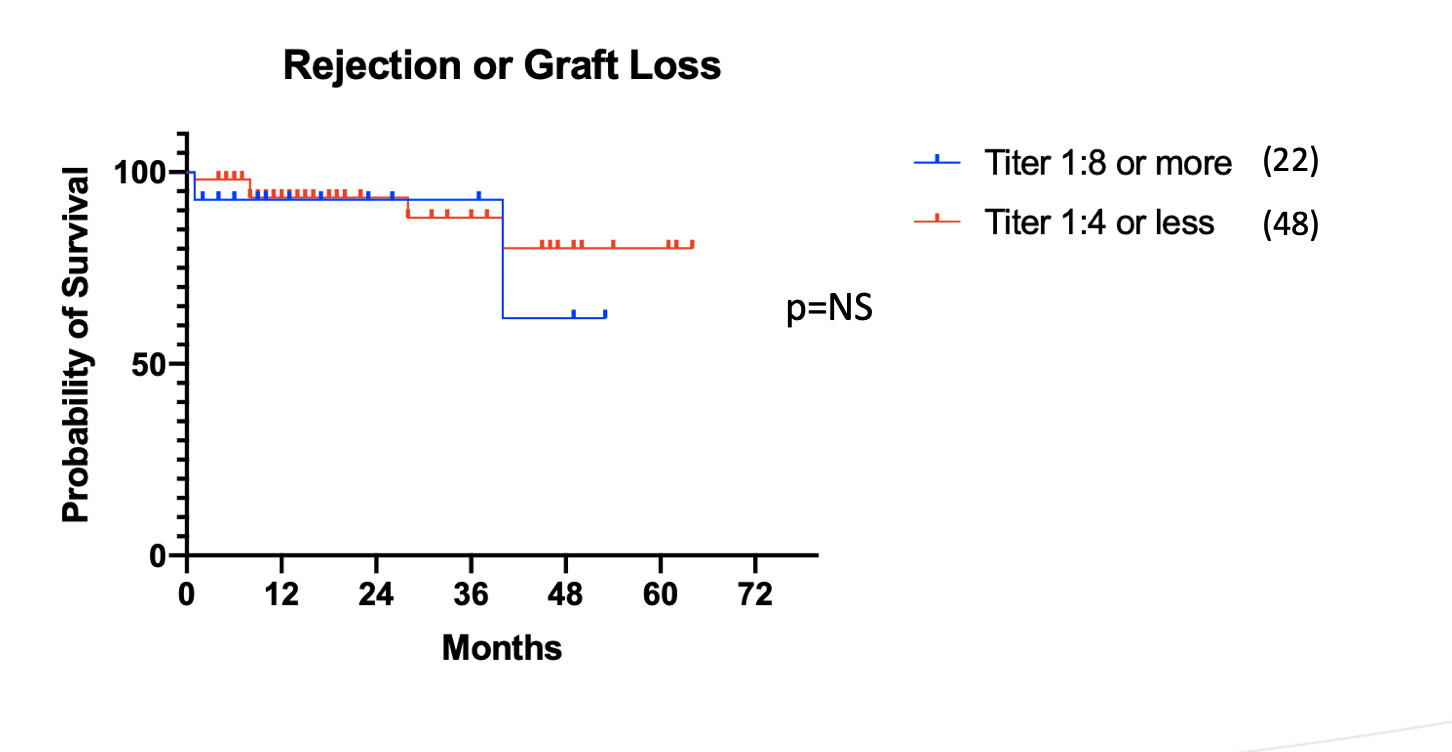
*Methods: This is a single center retrospective study. We reviewed all patients who received kidneys from donors across minor ABOi. At our center, these patients are transplanted using our standard protocol including induction with lymphodepleting antibodies and a maintenance regimen of tacrolimus and mycophenoloic acid. No plasmapheresis or other treatment was given to any patient regardless of titer. Recipients were classified as having either high anti-A2 titers (1:8 or greater) or low anti A2 titers (1:4 or less). Outcomes included graft loss and biopsy proven rejection as well as 3 month and 12 month serum creatinine. Outcomes were evaluated using Kaplan-Meier plots compared with the Mantel-Cox long rank test.
*Results: Since December of 2014 we performed a total of 70 transplants across minor ABOi. These included 56 deceased donor transplants from A2 or A2B donors into blood group B recipients, 14 living donor A2/A2B to group B transplants, and 10 living donor A2/A2B transplants into O recipients. Of these, 22 were high titer: 1:8 (n=11), 1:16 (n=6), 1:32 (n=5) and 48 were low titer. Follow up was similar in each group with mean follow up of 20 months in the high titer group (range 3-40 months) and 21 months in the low titer group (range 3-54 months). There was no statistically significant difference in graft survival (figure 1) between the groups, nor was there a statistically significant difference in the composite endpoint of rejection or graft loss (figure 2). At 3 months, serum creatinine was similar between the groups (median 1.41 vs 1.42, mean 1.58 vs 1.52, p=ns). 12 month serum creatinine was also statistically similar (median 1.47 vs 1.27, mean 1.58 vs 1.52 p=ns).
*Conclusions: With modern immunosuppression, high-titer recipients show excellent results which are fully equivalent to results in low titer recipients of minor ABOi transplants.
To cite this abstract in AMA style:
Gilbert A, Radomski S, Verbesey J, Vucci J, Cooper M. Expanding A2 to B Kidney Transplantation: Safe and Effective Use of Recipients with High Titer Antibodies [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/expanding-a2-to-b-kidney-transplantation-safe-and-effective-use-of-recipients-with-high-titer-antibodies/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress