Effect of Intrapatient Variability and Mean Tacrolimus Levels in Renal Transplant Patients
D. Goodall, M. Willicombe, A. McLean, D. Taube.
Imperial College Renal and Transplant Centre, Hammersmith Hospital, London, United Kingdom.
Meeting: 2015 American Transplant Congress
Abstract number: 500
Keywords: Immunosuppression, Kidney transplantation
Session Information
Session Name: Concurrent Session: Psychosocial and Treatment Adherence
Session Type: Concurrent Session
Date: Tuesday, May 5, 2015
Session Time: 4:00pm-5:30pm
 Presentation Time: 4:48pm-5:00pm
Presentation Time: 4:48pm-5:00pm
Location: Room 121-C
Introduction
Nonadherence (NA) to immunosuppressive medication and adherence to immunosuppressive protocols is a potent risk factor for rejection and graft loss, which can be both patient and / or physician led. We have previously shown that intrapatient variability (IPV) of tacrolimus trough levels can predict rejection and graft loss. In this study, we link IPV with the maintenance of subtherapeutic, therapeutic and supratherapeutic tacrolimus trough levels.
Method
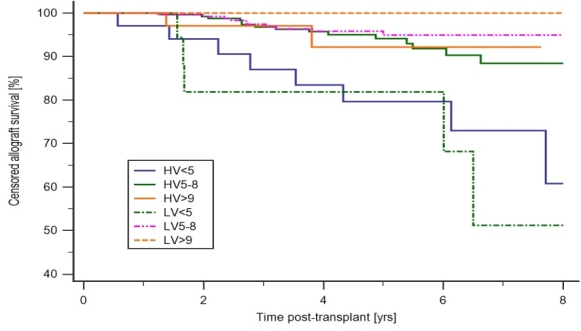
We retrospectively analysed 668 patients who received a kidney only transplant between 01/11/2005 and 01/09/2013. All patients received alemtuzumab induction and tacrolimus monotherapy with a steroid sparing protocol with a target pre-trough tacrolimus level of 5-8ng/ml. Coefficient of variance (COV) was defined as standard deviation/mean of all outpatient tacrolimus trough levels taken between 6 and 12 months post-transplant. High variability (HV) was defined as a COV>median of the overall cohort and low variability (LV) was defined as a COV ≤ median of the overall cohort.
Results
5983 tacrolimus levels were included in the analysis. The mean number of samples analysed per patient was 8.96 ± 3.78 The median coefficient of variance of tacrolimus levels was 18.15% (range 1.3 – 86.3)
Graft survival was 51.2% and 94.9% in the LV<5ng/ml and LV 5-8ng/ml group respectively p<0.0001
AMR free survival was 80% and 97.5% in the LV<5ng/ml and LV 5-8ng/ml group respectively p<0.0001
TG free survival was 74.8% and 98% in the LV<5ng/ml and LV 5-8ng/ml group respectively p<0.0001.
Figure 1 shows that allograft survival was significantly poorer in the patients with subtherapeutic tacrolimus levels, irrespective of the IPV of their tacrolimus levels.
Conclusion
This study shows that patients maintained on a minimalist tacrolimus monotherapy regimen post kidney transplant are most at risk of developing AMR, TG and graft loss if their tacrolimus levels are < 5ng/ml, especially if the tacrolimus COV is low . Raising the tacrolimus dose to maintain levels between 5-8ng/ml is very important unless there are good mitigating clinical reasons.
To cite this abstract in AMA style:
Goodall D, Willicombe M, McLean A, Taube D. Effect of Intrapatient Variability and Mean Tacrolimus Levels in Renal Transplant Patients [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/effect-of-intrapatient-variability-and-mean-tacrolimus-levels-in-renal-transplant-patients/. Accessed February 17, 2026.« Back to 2015 American Transplant Congress
