Early Sub-Clinical and Clinical TCMR Are Associated with Progressive Renal Allograft Dysfunction
UPMC, Pittsburgh.
Meeting: 2018 American Transplant Congress
Abstract number: D185
Keywords: Rejection
Session Information
Session Name: Poster Session D: Kidney: Acute Cellular Rejection
Session Type: Poster Session
Date: Tuesday, June 5, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: The clinical course and significance of early sub-clinical (SCR) and clinical TCMR (ACR) vs. no rejection (NR) is unclear. In this prospective study, we have systematically analyzed early SCR, ACR and NR in relation to their histological progression and clinical course.
Methods: We routinely perform 2 protocol Bx (3 & 12mo) along with any for-cause Bx through the 1st post-transplant yr. 294/372 patients (dates: 01-13 to 11-14) underwent at least one Bx and are included in this analysis. Of these patients, 14% had SCR whilst 10.5% had clinical TCMR (ACR) in the early post-transplant period (0-4mos). We analyzed the impact of SCR and ACR with reference to subsequent TCMR, 1-year allograft chronicity as well as graft loss or impending graft loss (eGFR<30ml/min with >30% decline from baseline) at 4yrs in comparison to the NR group.
Results: Patients with SCR and ACR had a higher chance of late, persistent or recurrent AR despite therapy (p=0.02) (Fig 1A). Patients with SCR and ACR had worse chronic histological changes (IFTA) noted on the 1yr protocol Bx (Fig 1B) (p=0.009). Both SCR and ACR groups had a
significantly worse composite endpoint of graft loss or impending graft loss at 4yrs in comparison to the NR group (p<0.01) (Fig 1C). In contrast, the graft outcome was similar among patients with SCR and ACR groups (p=NS). Subset of patients with persistent or recurrent TCMR based on early SCR (p=0.08) and ACR (0.007) had significantly worse outcome despite standard of care therapy with corticosteroids. Logistic regression analysis showed that DCD donor source (OR 5.95, p=0.03) and post-transplant DSA (OR 3.1, p=0.05) were risk variables for persistence or recurrence of late TCMR.
Conclusion: In conclusion, patients with early sub-clinical and Clinical TCMR have significantly worse graft outcomes (allograft chronicity at 1year and impending graft loss) in comparison to those without TCMR. Further, both early SCR and ACR had comparable graft outcomes. In both these groups a significant proportion of patients have persistent or recurrent late TCMR despite therapy and these patients have worse clinical outcome in comparison to those who respond to therapy.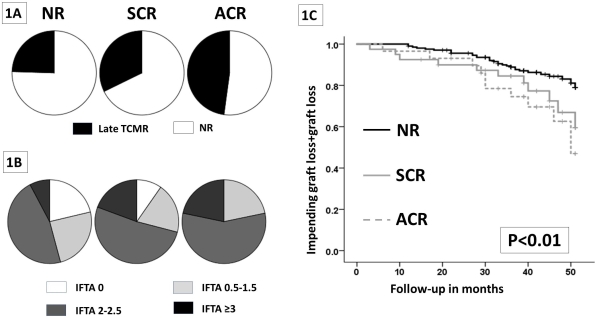
CITATION INFORMATION: Cherukuri A., Chittka D., Mehta R., Sood P., Hariharan S. Early Sub-Clinical and Clinical TCMR Are Associated with Progressive Renal Allograft Dysfunction Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Cherukuri A, Chittka D, Mehta R, Sood P, Hariharan S. Early Sub-Clinical and Clinical TCMR Are Associated with Progressive Renal Allograft Dysfunction [abstract]. https://atcmeetingabstracts.com/abstract/early-sub-clinical-and-clinical-tcmr-are-associated-with-progressive-renal-allograft-dysfunction/. Accessed February 16, 2026.« Back to 2018 American Transplant Congress
