Early Rejection in the Elderly: Is It Predictable?
University of Maryland Medical Center, Baltimore, MD
Meeting: 2017 American Transplant Congress
Abstract number: B189
Keywords: Elderly patients, HLA matching, Rejection, Simulect
Session Information
Session Name: Poster Session B: Kidney Immunosuppression: Induction Therapy
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Introduction: Optimal induction for elderly kidney transplant recipients (KTR) remains unclear. Older age may be associated with decreased immunogenicity; however, clinical heterogeneity of the elderly is unpredictable. While lymphocyte depleting therapy in elderly has been associated with escalating risk of death and graft loss, non-depleting induction has led to increased rejection. The purpose of this case-controlled study was to identify which immunologic risk factors, such as number of HLA mismatches and percent panel-reactive antibody (PRA), are associated with early rejection in KTR >65 years old.
Methods: A retrospective chart review was conducted of first time KTR >65 receiving basiliximab induction from 2008-2016 who experienced biopsy-proven acute rejection (BPAR) requiring treatment within 6 months post-transplant. The 50 patients identified were matched in a 2:1 fashion to patients >65 who received basiliximab and were rejection-free in the first 6 months according to race, transplant type, sex, and age. All patients were started on maintenance immunosuppression (IS) of tacrolimus goal 6-8ng/mL, mycophenolate equivalent of 2000mg/day, and a steroid taper. Subgroup analysis of BPAR at 3 months was performed to better correlate with pharmacokinetic properties of basiliximab.
Results: There were no differences in baseline demographics. Donor risk factors, including age, sex, race, kidney donor profile index, donor after cardiac death, cold ischemic time, and T and B flow crossmatch, were successfully controlled. There were no differences in recipient factors of primary disease, comorbidities, delayed graft function, or maintenance IS. There was no difference in HLA mismatches or PRA at 6 months. Subgroup analysis demonstrated an association with increased HLA mismatches and BPAR at 3 months.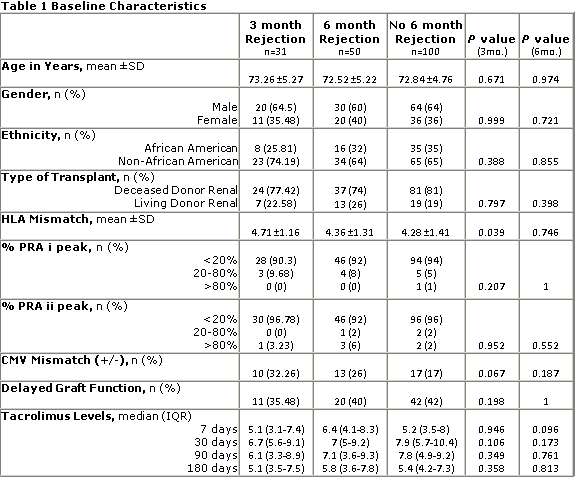 Conclusion: HLA mismatch was a risk factor for BPAR at 3 months post-transplant, suggesting use of more potent induction in this population. HLA mismatches and PRA were not risk factors for early BPAR or graft survival at 6 months post-transplant in KTR >65 years old. Further investigation is required to explore effects of class I and class II HLA mismatches.
Conclusion: HLA mismatch was a risk factor for BPAR at 3 months post-transplant, suggesting use of more potent induction in this population. HLA mismatches and PRA were not risk factors for early BPAR or graft survival at 6 months post-transplant in KTR >65 years old. Further investigation is required to explore effects of class I and class II HLA mismatches.
CITATION INFORMATION: Clark J, Sparkes T, Masters B, Jonchhe S, Haririan A, Thomas B, Ravichandran B. Early Rejection in the Elderly: Is It Predictable? Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Clark J, Sparkes T, Masters B, Jonchhe S, Haririan A, Thomas B, Ravichandran B. Early Rejection in the Elderly: Is It Predictable? [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/early-rejection-in-the-elderly-is-it-predictable/. Accessed March 4, 2026.« Back to 2017 American Transplant Congress
