Early Impact of the New United Network for Organ Sharing Simultaneous Liver-Kidney Transplantation Allocation Policy: Improved Standardization but Similar Utilization
1UCSF, San Francisco, CA, 2Columbia University, New York, NY
Meeting: 2019 American Transplant Congress
Abstract number: 552
Keywords: Kidney/liver transplantation, Liver cirrhosis, Renal dysfunction, Renal failure
Session Information
Session Name: Concurrent Session: Liver - Kidney Issues in Liver Transplantation
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: Room 302
*Purpose: In an effort to standardize SLKT utilization, UNOS/OPTN implemented a new SLKT policy on August 10th, 2017. We aimed to characterize the early impact of this policy change on listing for SLKT, SLKT transplantation, and early post-SLKT renal/overall survival.
*Methods: UNOS data for all non-status 1 adult (≥18y) patients listed for LT from 8/10/16 – 11/10/17 were analyzed. To determine the impact of the SLKT policy change, we compared LT candidates in the following periods based on either their listing (to compare listing characteristics) or transplant date (to compare transplant recipient characteristics): Era 1 (8/10/16-11/10/16); Era 2 (5/10/17-8/10/17); Era 3 (8/10/17-11/10/17). We then determined the primary outcome, a composite of either 90d-renal graft failure (RF) (as reported to UNOS, at 90 days post-DDRT, not including mortality) or 90d-mortality, by era of SLKT. Cox-regression clustered on center then determined the association between the period of SLKT and the primary outcome.
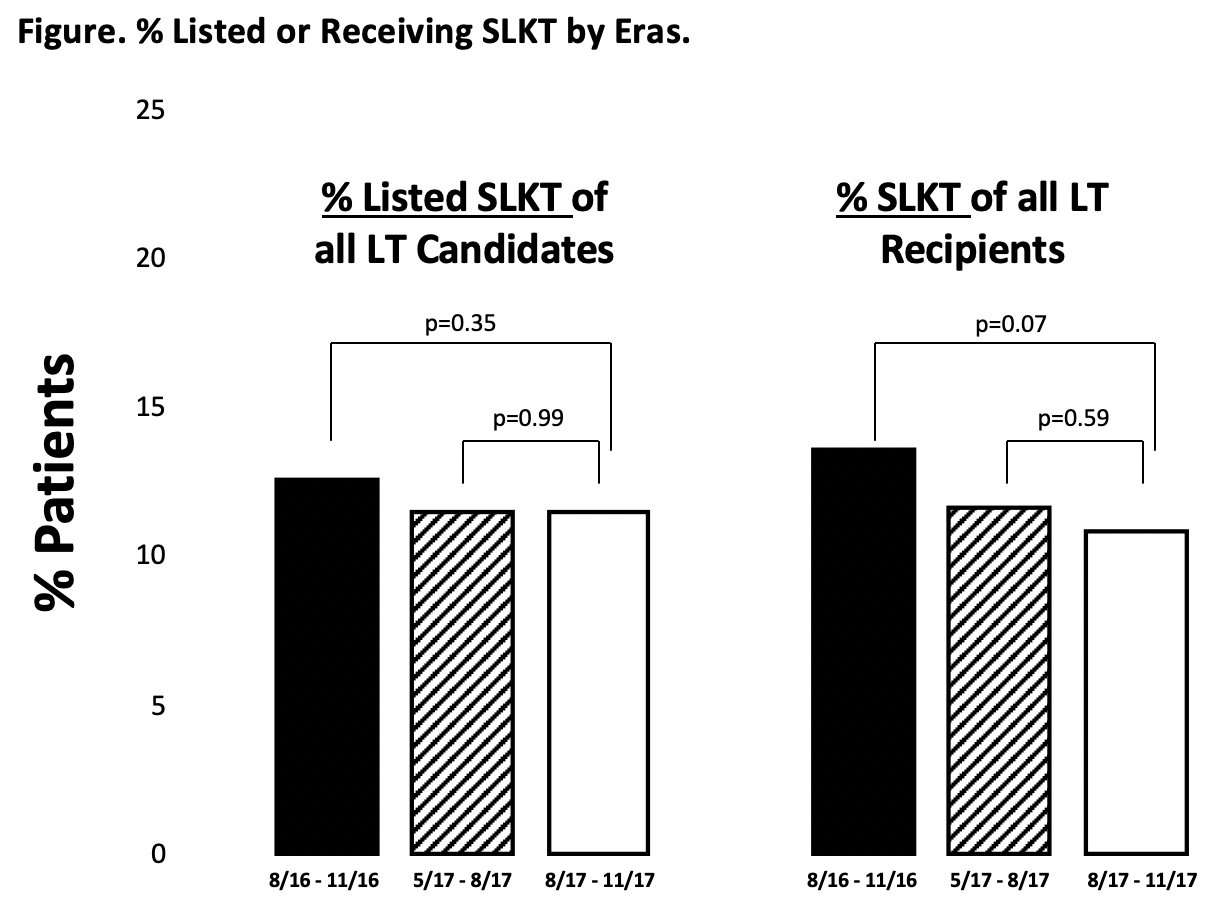
*Results: There were 1621 patients listed in Era 1, 1672 in Era 2, and 1623 in Era 3. There were no significant differences in the % of patients listed for SLKT between the listing eras: Era 1: 13% v. Era 2: 12% v. Era 3: 12% (p=0.56) (Figure). There were 969 LT recipients in Era 1, 1018 in Era 2, and 997 in Era 3. There were no significant differences in the % of patients who underwent SLKT between the transplant eras: Era 1: 14% v. Era 2: 12% v. Era 3: 11% (p=0.17) (Figure). As compared to SLKT recipients before the policy change, SLKT recipients who underwent transplant after the policy change were more likely to meet the UNOS SLKT criteria (Era 3: 62% v. Era 1: 48% v. Era 2: 47%, p=0.045). Otherwise, there were no differences between the eras, including median KDPI among SLKT recipients by transplant period: Era 1: 39% v. Era 2: 36% v. Era 3: 36% (p=0.97). There were 132 SLKT recipients in Era 1, 119 SLKT recipients in Era 2, and 109 SLKT recipients in Era 3. There were no significant differences in the % 90d-RF/mortality in each era among SLKT recipients: Era 1: 8% v. Era 2: 7% v. Era 3: 8% (p=0.87). In cox-regression analysis, SLKT after implementation of the new policy was not associated 90d-RF/mortality: as compared to Era 3, Era 1: HR 1.0(95CI 0.3-2.9), Era 2: HR 1.1(0.4-3.1).
*Conclusions: There were no significant changes in the % of patients listed for or % of patients who received a SLKT after implementation of the new policy. There were no differences in 90-RF/mortality after implementation of the new policy. Further follow-up is needed to determine the long-term impact of the new SLKT allocation policy.
To cite this abstract in AMA style:
Cullaro G, Verna EC, Lai JC. Early Impact of the New United Network for Organ Sharing Simultaneous Liver-Kidney Transplantation Allocation Policy: Improved Standardization but Similar Utilization [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/early-impact-of-the-new-united-network-for-organ-sharing-simultaneous-liver-kidney-transplantation-allocation-policy-improved-standardization-but-similar-utilization/. Accessed February 27, 2026.« Back to 2019 American Transplant Congress