Early Complications after ABO Incompatible Kidney Transplantation: A National Database Study
Saint Louis Univ
Dartmouth Univ
Johns Hopkins Univ,
Washington Univ
Meeting: 2013 American Transplant Congress
Abstract number: 154
ABO incompatible (ABOi) live donor kidney transplantation (LKDT) with plasmapheresis can achieve acceptable graft survival. However, intermediate outcomes after ABOi LDKT have not been described in multi-center cohorts. We examined United States Renal Data System registry data for Medicare-insured LDKT recipients in 2000-2007 (n=13,500) to study associations of ABOi LKDT with hemorrhage and infections in a nationally representative cohort.
ABOi (n=124) LDKTs were identified using donor and recipient ABO group reported to the national registry. A2-to-O (A2O, n =30) LDKTs were categorized separately, due to data that A2O transplant may be safe without additional treatment. Hemorrhage and infection events were identified by ICD-9 codes on billing claims. Associations of ABOi and A2O with complications 0-90 and 91-365 d post-transplant were assessed by Cox regression, with adjustment for recipient, donor and transplant factors in the UNOS Kidney Allocation Review Committee model.
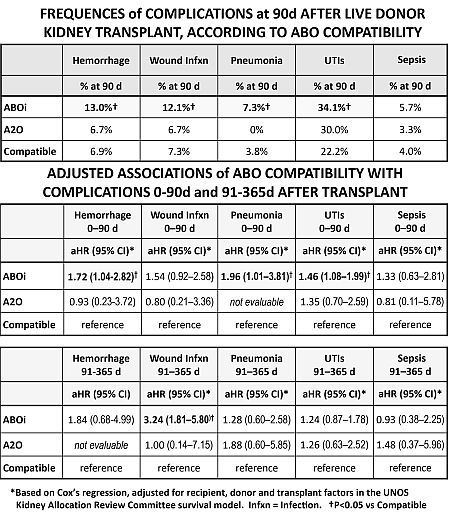
Unadjusted complication frequencies at 90d among recipients of ABOi vs compatible LDKT were significantly higher for hemorrhage, 13.0% vs 6.7%; wound infections, 12.1% vs 7.3%; pneumonia, 7.3% vs 3.8%; and UTIs, 34.1% vs 22.2%, respectively (Table 1). In multivariate regression, ABOi was associated with nearly twice the relative risk of pneumonia (aHR 1.97), 72% higher risk of hemorrhage, and 46% higher risk of UTIs over 0-90d (Table 2). Adjusted risk of wound infections was >3-times higher (aHR 3.24) for ABOi vs compatible LKDT at 91-365d post-transplant, while risks of other complications in this period did not vary by ABO compatibility. Sepsis was not significantly associated with ABOi, and A2O LKDT was not associated with risk of any complications.
ABOi LKDT offers patients with potential live donors an additional transplant option, but with higher risks of early post-transplant bleeding and infections. The risk period for wound infections may extend longer. Further work should evaluate the importance of complications in the cost effectiveness of ABOi LDKT.
To cite this abstract in AMA style:
Lentine K, Axelrod D, Simpkins C, Xiao H, Tuttle-Newhall J, Schnitzler M, Dharnidharka V, Brennan D, Segev D. Early Complications after ABO Incompatible Kidney Transplantation: A National Database Study [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/early-complications-after-abo-incompatible-kidney-transplantation-a-national-database-study/. Accessed February 16, 2026.« Back to 2013 American Transplant Congress
