Durable Clinical and Immunologic Advantage of Living Donor Liver Transplantation (LDLT) in Children.
E. Przybyszewski,1 S. Lobritto,1 M. Martinez,1 J. Vittorio,1 A. Fox,1 B. Samstein,2 T. Kato,1 A. Griesemer,1 J. Emond.1
1Columbia University Medical Center, New York, NY
2Weill Cornell Medical College, New York, NY.
Meeting: 2016 American Transplant Congress
Abstract number: 237
Keywords: Liver grafts, Living-related liver donors, Pediatric, Rejection
Session Information
Session Name: Concurrent Session: Living Donor Liver Transplantation
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: Room 210
Purpose:
Despite good results, only 10% of liver transplants in children in the US are from living donors. In addition to optimal timing and graft quality, LDLT may offer immunologic advantage since most donors are haplo-identical parents. In this single center study we sought to quantify the benefit of LDLT with granular outcomes over the longterm.
Methods:
Data were collected on 250 children (n=184 DD, n=66 LD) surviving at least 1-year with up to 18-years of followup. LD and DD were compared with respect to demographics, graft type, rejection, immunosuppression (IS), complications, and graft failure; analyzed using SPSS.
Results:
DD recipients were older (5.9±6.5y vs 4.1±5.5y, p=0.039) with less followup (6.7±4.3y vs 9.0±5.3y, p=0.001). Compared to DD, LD recipients had lower maximum BANFF scores (3.7±2.3 vs 5.1±2.0, p<0.0001), fewer steroid recycles (1.1±1.1 vs 1.7±1.5, p=0.003), were more likely to be free of acute rejection (27% vs 15%, p=0.03), less likely to have chronic rejection (4.5% vs 13.6%, p=0.046), and more likely to be on monotherapy or off IS (85% vs 55%, p<0.00001). Mean tacrolimus levels in the last year of followup were LD:3.39±1.13 vs DD:4.52±1.65, p=0.004. Overall LD patients had a trend to higher graft survival (p=0.057, Fig 1).
To adjust for differences in patient characteristics, we performed a subgroup analysis of biliary atresia patients (n=80 DD, n=43 LD). Here, LD recipients had less chronic rejection (0% vs 12.5%, p=0.016), lower maximum BANFF scores (3.8±2.3 vs 4.9±1.9, p=0.009), were more likely to be on monotherapy or off IS (88% vs 68%, p=0.011). Graft survival was not significantly higher (p=0.09, Fig 2). However, biliary complications were doubled in LD (56% vs 28%, p=0.002).
Conclusion:
This study demonstrates the benefit of LDLT on multiple clinical parameters over longterm followup. The high rate of biliary complications, especially in LDLT, mandates aggressiveness to mitigate this treatable cause of chronic graft injury. Further study in larger populations will address the generalizability of these findings. 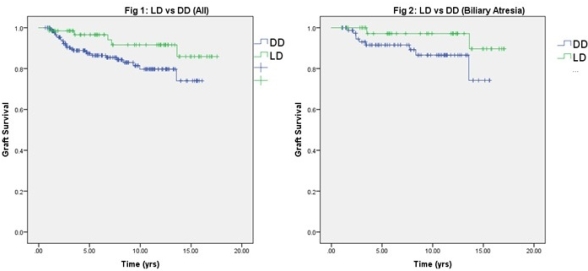
CITATION INFORMATION: Przybyszewski E, Lobritto S, Martinez M, Vittorio J, Fox A, Samstein B, Kato T, Griesemer A, Emond J. Durable Clinical and Immunologic Advantage of Living Donor Liver Transplantation (LDLT) in Children. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Przybyszewski E, Lobritto S, Martinez M, Vittorio J, Fox A, Samstein B, Kato T, Griesemer A, Emond J. Durable Clinical and Immunologic Advantage of Living Donor Liver Transplantation (LDLT) in Children. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/durable-clinical-and-immunologic-advantage-of-living-donor-liver-transplantation-ldlt-in-children/. Accessed March 2, 2026.« Back to 2016 American Transplant Congress
