DSA with TCMR Identifies High Risk Renal Transplant Recipients That Can Be Predicted by Proinflammatory Transitional B Cells
Starzl Transplant Inst., Univ. of Pittsburgh, Pittsburgh.
Meeting: 2018 American Transplant Congress
Abstract number: 500
Keywords: Antibodies, Rejection
Session Information
Session Name: Concurrent Session: Biomarkers, Immune Monitoring and Outcomes: Clinical
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Room 602/603/604
Post-transplant DSA is strongly associated with poor graft outcomes but has limited predictive value. In this prospective study we aimed to risk-stratify patients with early post-transplant DSA to allow timely identification of individuals at risk for poor clinical outcomes. Patients were screened for DSA at 0,1,3,6,9 &12mo and analyzed in relation to protocol biopsies at 3 and 12mos and any for-cause biopsies within the first year. IS was with Thymo and MPA+TAC.
67/294 (22.8%) of patients transplanted (1/2013-11/2014) developed DSA. DSA was detected early (<3mo) in 76% of the patients. DSA was associated with significantly increased rates of subclinical and clinical TCMR (58%) compared to patients lacking DSA (33%, %; p<0.0001). Importantly, patients with DSA+TCMR had significantly worse chronic allograft changes (1yr protocol Bx) and increased graft loss or impending graft loss (eGRF<30ml/min and >30% fall from baseline) at 4yrs compared to those with DSA or TCMR alone (Fig1A). Thus, DSA+TCMR identifies high-risk patients, in whom early identification would allow pre-emptive intervention. Based on prior findings, we asked whether cytokine expression by peripheral blood B cell subsets could predict TCMR in patients with DSA. 43/67 DSA+ patients had their B cell cytokines analyzed at 3mo. Of markers analyzed, the ratio of IL-10/TNFα expression by T1 transitional B cells was significantly lower in patients with DSA+TCMR compared to those with DSA alone (ratio: 0.94 vs. 4.9, p<0.0001). A low T1B cytokine ratio was a strong predictor of DSA+TCMR (ROC AUC 0.94, p<0.0001; Fig 1B). At a cut-off value of 1.26, the T1B cytokine ratio predicted DSA+TCMR with a PPV of 81% and a NPV of 94%. Reanalysis of the data after removing the 5/43 patients whose DSA was detected after TCMR showed that the T1 B cytokine ratio strongly predicted concomitant or ensuing TCMR in patients with DSA (ROC AUC 0.94, p<0.0001). Thus, patients with DSA+TCMR represents a high-risk population for adverse graft outcomes, and this outcome can be predicted in DSA+ patients using the T1B cytokine ratio as a biomarker. 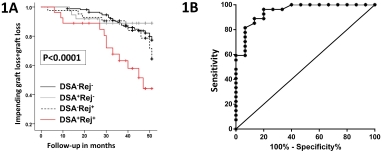
CITATION INFORMATION: Chittka D., Cherukuri A., Sharma A., Mehta R., Hariharan S., Rothstein D. DSA with TCMR Identifies High Risk Renal Transplant Recipients That Can Be Predicted by Proinflammatory Transitional B Cells Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Chittka D, Cherukuri A, Sharma A, Mehta R, Hariharan S, Rothstein D. DSA with TCMR Identifies High Risk Renal Transplant Recipients That Can Be Predicted by Proinflammatory Transitional B Cells [abstract]. https://atcmeetingabstracts.com/abstract/dsa-with-tcmr-identifies-high-risk-renal-transplant-recipients-that-can-be-predicted-by-proinflammatory-transitional-b-cells/. Accessed February 19, 2026.« Back to 2018 American Transplant Congress
