Donation after Cardiac Simultaneous Liver-Kidney: An Updated Perspective
Mayo Clinic AZ, Phoenix, AZ
Meeting: 2019 American Transplant Congress
Abstract number: 556
Keywords: Donors, marginal, Donors, non-heart-beating, Kidney/liver transplantation
Session Information
Session Name: Concurrent Session: Liver - Kidney Issues in Liver Transplantation
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Room 302
*Purpose: Historically, the outcomes from donation after cardiac death (DCD) donors have been shown to be inferior as compared to those of donation after brain death (DBD) donors. More recent data has shown improvement in these outcomes. Nonetheless, DCD organs continue to be underutilized and the use of DCD donors for simultaneous liver-kidney (SLK) recipients remains controversial. In order to investigate this in more detail, we compared outcomes of DBD and DCD SLK recipients.
*Methods: Between 2004 and 2018, 74 SLK recipients from Mayo Clinic Arizona were identified. We began doing DCD SLK in 2014. Results were analyzed using chi-square, unequal variance t-tests and Kaplan-Meier survival analysis.
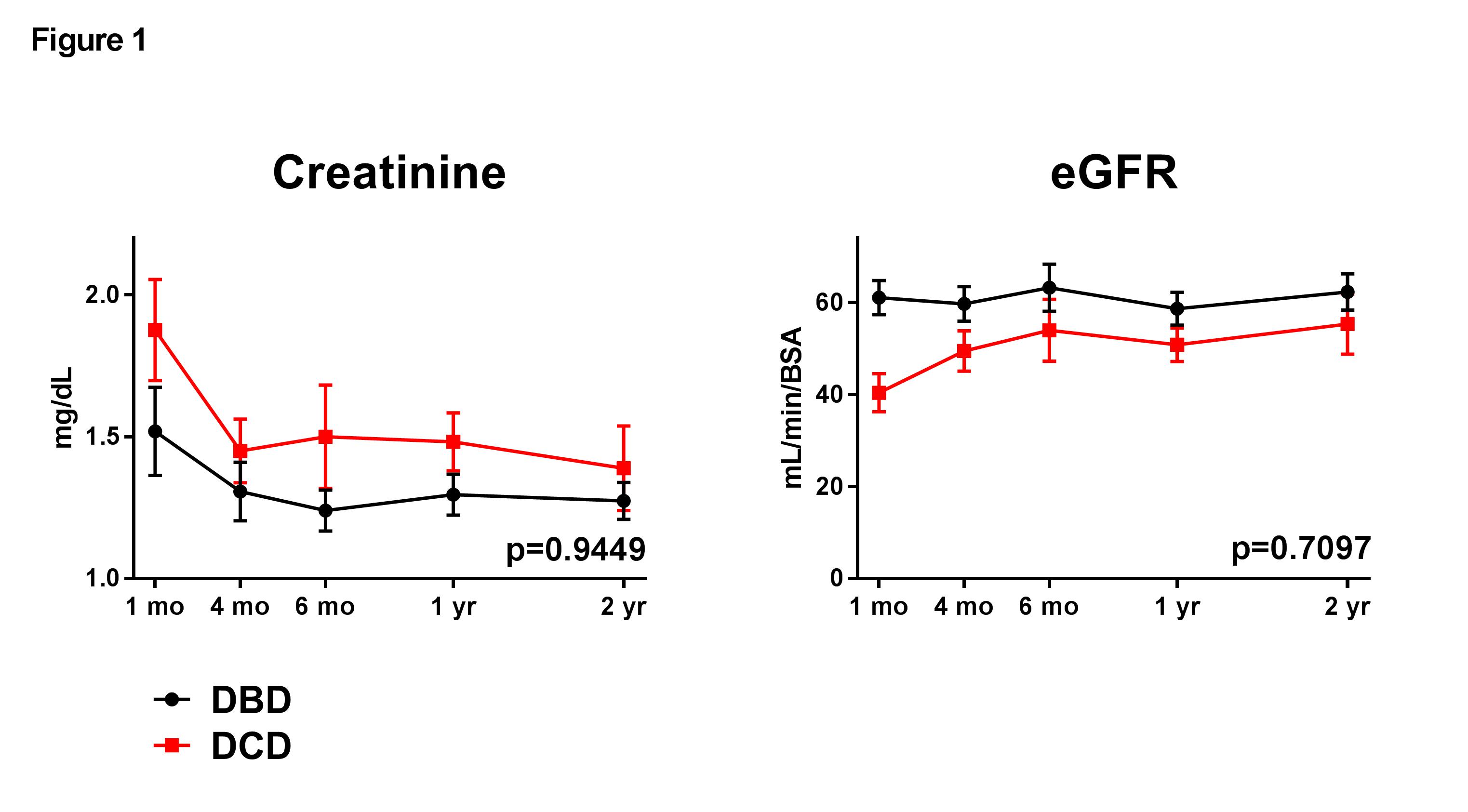
*Results: 53 (71.6%) SLK were from DBD donors; 21 (28.4%) were from DCD donors. In comparing DBD and DCD SLK groups, no differences were observed in recipient age (p=0.6149), biologic MELD (26.7±7.5 vs. 23.6±6.3, p=0.0957), or primary liver disease (p=0.3161). The majority of DBD and DCD SLK recipients were on dialysis prior to transplant (73.6% vs. 61.9%, p=0.2695). There were no differences in liver (p=0.2119) or kidney (p=0.7861) allograft cold ischemia times. DCD donor warm ischemia time was 22.1±5.0 minutes. There were no differences in the kidney donor profile index (KDPI) between DBD and DCD groups (37.2%±25.8% vs. 47.9%±23.8%, p=0.1142). Post-SLK, there was more delayed graft function (DGF) in the DCD cohort (57.1% vs. 29.5%, p=0.0118). For those with DGF, there were no differences between DBD and DCD groups with the time spent on dialysis (days) (p=0.1856) or hospital length of stay (p=0.7347). There were no long-term differences in creatinine (p=0.9449) or eGFR (p=0.7097) at 1 and 2 years between DBD and DCD SLK groups (Figure 1). There were no differences in patient (p=0.3669), liver allograft (p=0.9675), or kidney allograft (p=0.9090) survival (Figure 2).
*Conclusions: With experience, good outcomes can be achieved with DCD SLK transplants. Consideration should be given for using DCD donors for SLK recipients with lower MELD scores who are otherwise disadvantaged in organ allocation. The use of DCD donors for SLK transplants affords the opportunity to obtain good quality kidney allografts.
To cite this abstract in AMA style:
Nunez R, Morgan P, Mathur A, Reddy KS, Moss A, Aqel B, Jadlowiec C. Donation after Cardiac Simultaneous Liver-Kidney: An Updated Perspective [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/donation-after-cardiac-simultaneous-liver-kidney-an-updated-perspective/. Accessed February 27, 2026.« Back to 2019 American Transplant Congress