Do Donor Specific Antibodies Affect Graft Liver Outcomes after Living Donor Liver Transplantation?
Department of Surgery, Yonsei University College of Medicine, Seoul, Republic of Korea
Meeting: 2013 American Transplant Congress
Abstract number: 111
Background: Preformed circulating donor specific antibodies (DSAs) immunologically challenge vascular endothelium and the bile duct. However, the liver is an immune tolerant organ and can avoid immunologic challenges. This study was undertaken to analyze the effects of DSAs after adult living donor liver transplantation (LDLT).
Patients and Methods: The medical records of 219 patients underwent LDLT between June 2006 and August 2012 were retrospectively reviewed and analyzed according to the presence of DSAs.
Results: Of the 219 patients, 32 (14.6%) showed the presence of DSAs and 187 (85.4%) did not. Class I DSAs were present in 11 patients, class II in 7, and both in 7 patients. Seven patients (3.2%) showed DSA to HLA-A, four (1.8%) to HLA-B, seven (3.2%) to HLA-DR, and 14 (6.4%) to two or more HLAs.
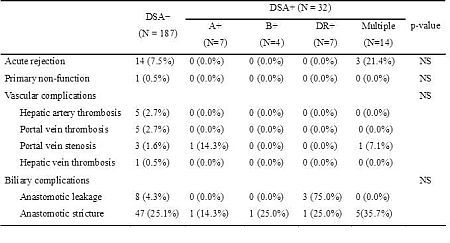
Pre-transplant clinical features in patients with or without DSAs were not different. However, female recipients showed more DSAs than male recipients in the DSA+ group. In addition, the DSA+ group showed significantly higher levels of both panel reactive antibody (PRA) class I and II than the DSA− group. No significant intergroup differences were found between incidences of primary non-function, acute rejections, vascular complications, or biliary complications. In addition, graft survival rates in the two groups showed no significant difference. However, the recipients with multiple DSAs tended to have more acute rejection episodes, a more events of biliary stricture, and a lower graft survival rate than patients in the DSA- group.
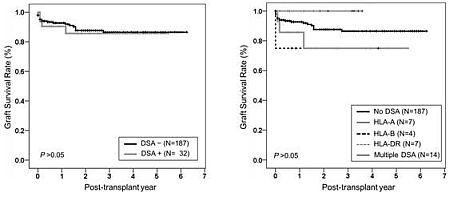
Conclusion: In LDLT, the presence of DSAs did not affect graft outcome measures, such as, acute rejection, vascular or biliary complications, and graft survival. However, the presence of multiple DSAs seems to be associated with poor graft outcomes.
To cite this abstract in AMA style:
Joo D, Song S, Lee S, Kim M, Lee A, Choi J, Kim S. Do Donor Specific Antibodies Affect Graft Liver Outcomes after Living Donor Liver Transplantation? [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/do-donor-specific-antibodies-affect-graft-liver-outcomes-after-living-donor-liver-transplantation/. Accessed February 6, 2026.« Back to 2013 American Transplant Congress
