Disparate Performance of Two Commonly Used Glomerular Filtration Rate Estimation Equations in Lung Transplant Patients
Nephrology &
Hypertension, Cleveland Clinic, Cleveland, OH
The Kidney Institute, Nephrology, Dialysis &
Transplantation, Houston, TX
Meeting: 2013 American Transplant Congress
Abstract number: B901
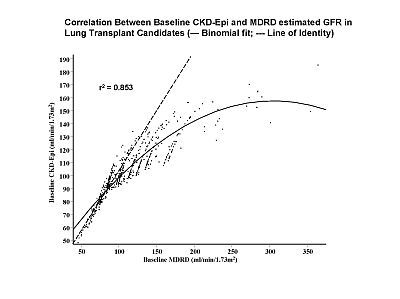
Purpose: The abbreviated Modification of Diet in Renal Disease (MDRD) and CKD-Epi equations employ the same variables (creatinine, race, gender) and are both commonly used to calculate estimated glomerular filtration rate (eGFR) before and after lung transplantation. A direct comparison of their performance in such patients has not previously been reported. Methods: We calculated baseline and one, six, and twelve month posttransplant eGFRs using both MDRD and CKD-Epi equations in a population of lung allograft recipients transplanted 1997 to 2009 and compared their performance at each time point. Results: 615 patients had baseline creatinine levels < 1mg/dl whereas 42 had baseline levels > 1mg/dl. Figure 1 shows the non-linear relationship of MDRD and CKD-Epi baseline eGFR (r2=0.853) despite each equation using identical variables. In those with baseline creatinine >1mg/dl the mean MDRD was 4 ml/min/1.73m2 lower than the mean CKD-Epi eGFR but in those with baseline creatinine <1mg/dl the mean MDRD eGFR was 11 ml/min/1.73m2 higher than the mean CKD-Epi eGFR (p<0.001). Due to the more pronounced overestimation of GFR by MDRD in those with more normal baseline renal function, the calculated loss of eGFR by 12 months post-transplant was higher when using MDRD vs. CKD-epi (-62+/-41 vs. -49+/-23 ml/min/1.73m2, p<0.001). Conclusions: Based on its more pronounced overestimation of GFR at normal levels of renal function the rate of loss of renal function after lung transplant appears more exaggerated using the MDRD vs. CKD-Epi equation. In the absence of more accurate measured GFR methodology, we recommend using the CKD-Epi equation to reduce bias.
To cite this abstract in AMA style:
Stephany B, Poggio E, Wehbe E. Disparate Performance of Two Commonly Used Glomerular Filtration Rate Estimation Equations in Lung Transplant Patients [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/disparate-performance-of-two-commonly-used-glomerular-filtration-rate-estimation-equations-in-lung-transplant-patients/. Accessed February 14, 2026.« Back to 2013 American Transplant Congress
