Critical Analysis of Death within 1 Year after Liver Transplantation, A
Abdominal Transplnatation, University of Arizona, Tucson
Meeting: 2013 American Transplant Congress
Abstract number: 544
Context: In the current era, 15% of liver transplant recipients die within the first year. While this may be viewed as a feat in comparison to waitlist morbidity and mortality, there is much room for improvement.
Objective: The objective of this analysis was to critically examine the mortality rates at differing time periods following liver transplantation to isolate high-risk periods. A further objective was to compare risk factors for mortality at these high-risk time periods.
Methods: We performed a retrospective analysis of UNOS de-identified patient-level data of all recipients of adult liver transplantation between January 1, 2002 and October 31, 2011. We analyzed 49,288 recipients. The primary outcome measure was patient death at 1 day, 30 days, and 365 days following liver transplantation. Multivariate logistic regression (stepwise backward) was performed.
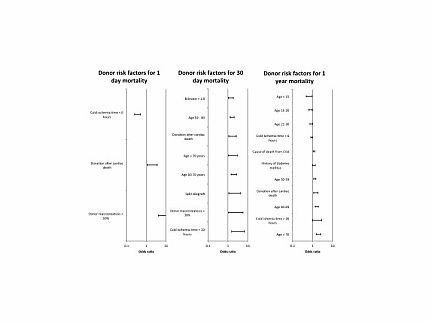
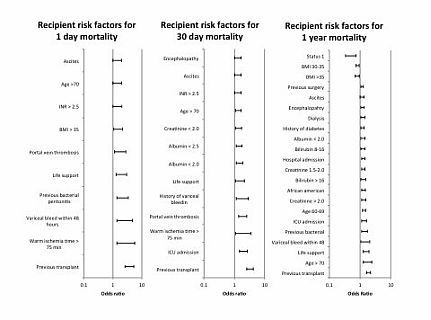
Results: The highest mortality rate was on Day 0 (.9%) followed by Day 1 (.5%). The first month had the highest mortality rate by month (3.5%). The first year had the highest mortality rate by year (16.1%). Figure 1 and 2 report the significant donor and recipient risk factors for 1 day, 1 month, and 1 year mortality. The strongest risk factors for 1 day mortality was donor macrosteatosis > 30% (OR 8.1 CI 4.1-15.9); 1 month mortality was previous transplant (OR 3.3 CI 2.6-4.2); and recipient age > 70 years (OR 2.0 CI 1.6-2.6).
Conclusion: The highest mortality rate after liver transplantation is after the first day, first month, and first year following liver transplantation. Each high-risk period has common and distinct risk factors for mortality. Previous transplant, macrosteatosis, and advanced recipient age were prominent risk factors.
To cite this abstract in AMA style:
Rana A, Porubsky M, Jie T, Habib S, Rilo H, Kaplan B, Gruessner A, Gruessner R. Critical Analysis of Death within 1 Year after Liver Transplantation, A [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/critical-analysis-of-death-within-1-year-after-liver-transplantation-a/. Accessed February 16, 2026.« Back to 2013 American Transplant Congress
