Covid-19 in Hiv-infected Solid Organ Transplant Recipients: A Case Series
M. Ramanathan, A. Fernandez, Y. Natori, J. Simkins, J. Camargo, M. Morris, N. Rivera, M. Loebe, G. Ciancio, L. Abbo, A. Mattiazzi, G. Guerra, S. Anjan
University of Miami, Miami, FL
Meeting: 2021 American Transplant Congress
Abstract number: 758
Keywords: HIV virus, Infection, Kidney/liver transplantation
Topic: Clinical Science » Infectious Disease » All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Coronavirus disease 2019 (COVID-19) is associated with increased mortality and morbidity in immunosuppressed patients. Data on management and outcomes in HIV-infected solid organ transplant (SOT) recipients is lacking.
*Methods: Single center, retrospective case series of HIV-infected SOT recipients who were diagnosed with COVID-19 by nasopharyngeal reverse transcriptase-polymerase chain reaction (RT-PCR) between April to November 2020. All patients had anti-retroviral therapy (ART) induced HIV viral load suppression at diagnosis.
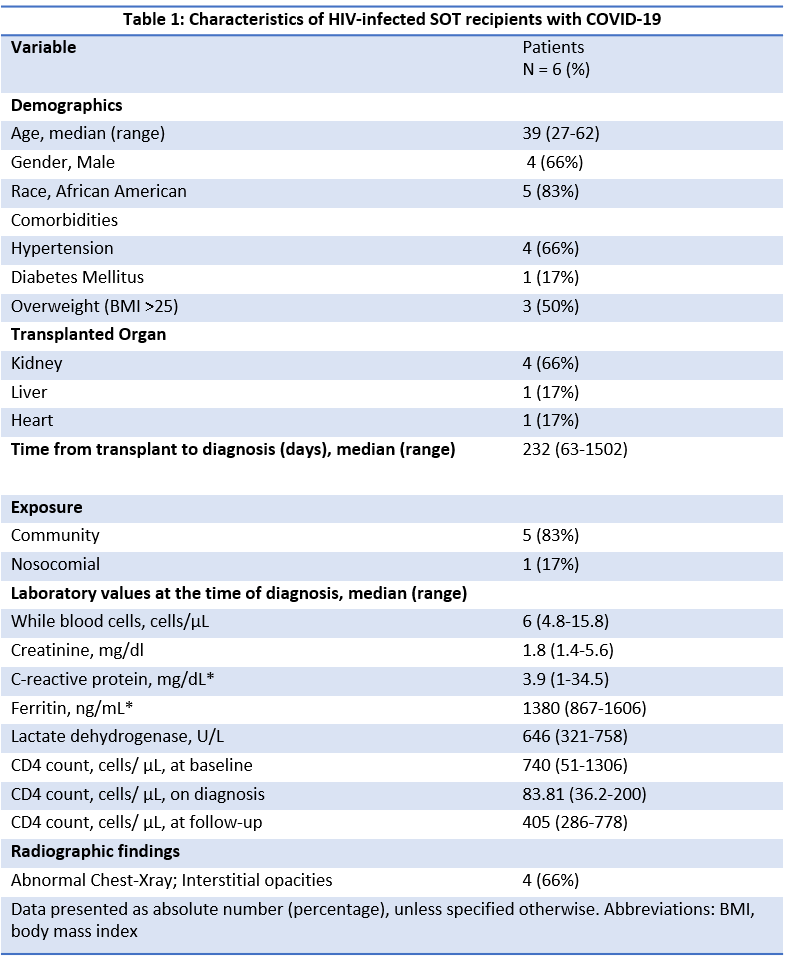
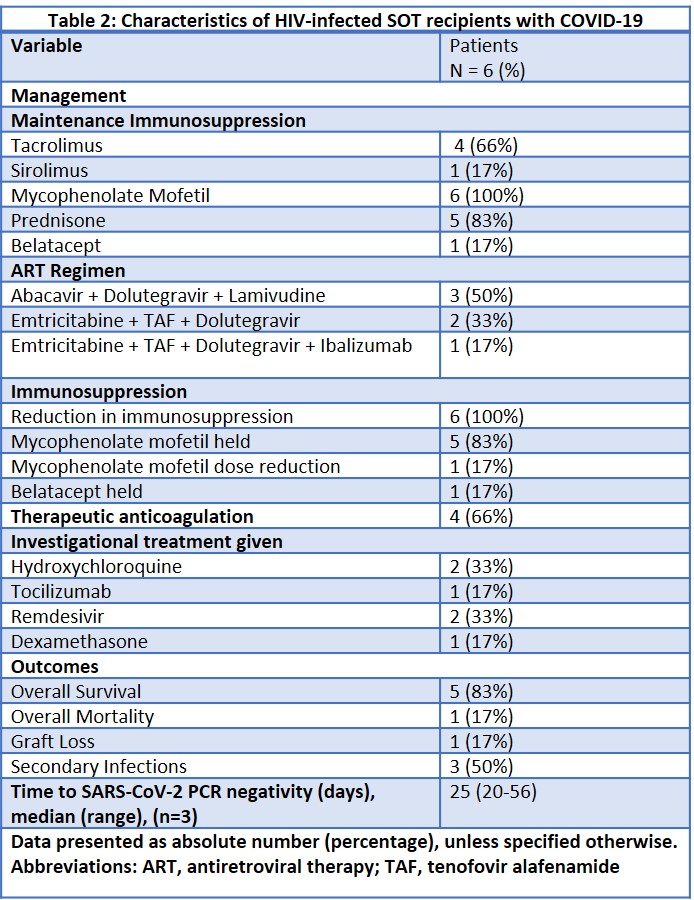
*Results: Six consecutive patients were identified (Table.1). Four patients required hospitalization; 2 were managed outpatient. Four were symptomatic with fever (75%), cough (50%), dyspnea (50%) and diarrhea (25%). An increase in inflammatory markers was seen in all patients, however only 4 (66%) required supplemental oxygen. Median time of follow up was 75 (range, 14-205) days. On diagnosis, first mycophenolate mofetil was discontinued or dose decreased by half. Calcineurin inhibitors and prednisone were continued. In addition, investigational therapies hydroxychloroquine, tocilizumab, remdesivir, dexamethasone were used in 3 (50%), 1 (17%), 1 (17%), 1 (17%), respectively (Table 2). All patients were on protease inhibitor sparing ART. A decrease in CD4 count from baseline was seen at the time of diagnosis which recovered over time. Overall, 5 (83%) survived, 1 (17%) died, 1 (17%) kidney transplant recipient had biopsy-proven acute T-cell mediated rejection 9 days after diagnosis with subsequent graft loss. Secondary infections were diagnosed with positive blood or respiratory cultures in 3 (50%). Death reported was due to septic shock from a secondary infection. Three patients had a negative SARS-CoV-2 RT-PCR at a median of 25 (range, 20-56) days from diagnosis.
*Conclusions: We report good outcomes in this unique, high risk cohort of HIV-infected SOT recipients. Balancing a decrease in immunosuppression and monitoring graft function to avoid graft loss is extremely important. Further studies are needed to determine the cumulative effect of HIV infection and organ transplant status on the severity of COVID-19.
To cite this abstract in AMA style:
Ramanathan M, Fernandez A, Natori Y, Simkins J, Camargo J, Morris M, Rivera N, Loebe M, Ciancio G, Abbo L, Mattiazzi A, Guerra G, Anjan S. Covid-19 in Hiv-infected Solid Organ Transplant Recipients: A Case Series [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/covid-19-in-hiv-infected-solid-organ-transplant-recipients-a-case-series/. Accessed February 23, 2026.« Back to 2021 American Transplant Congress