Covid-19 Impact of the Pandemic Surge on Patients Waiting for Renal Transplantation at a Single New York City Transplant Center
Transplant, NYP - Columbia University Medical Center, New York, NY
Meeting: 2021 American Transplant Congress
Abstract number: 204
Keywords: Kidney transplantation, Outcome, Outpatients
Topic: Administrative » Quality Assurance Process Improvement & Regulatory Issues
Session Information
Session Name: Quality Assurance and Regulatory Issues
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 7, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:45pm-4:50pm
Presentation Time: 4:45pm-4:50pm
Location: Virtual
*Purpose: There was a critical need to understand the impact that the COVID-19 pandemic had on our patients awaiting transplantation, including infection rates, morbidity, mortality, and wait list (WL) readiness.
*Methods: Retrospective single-center study of active kidney and pancreas WL patients. Clinicians called patients using a questionnaire to assess patient status, screen for COVID-19 symptoms and exposures, assess changes to psychosocial demographics, and instruct patients who needed follow-up care.
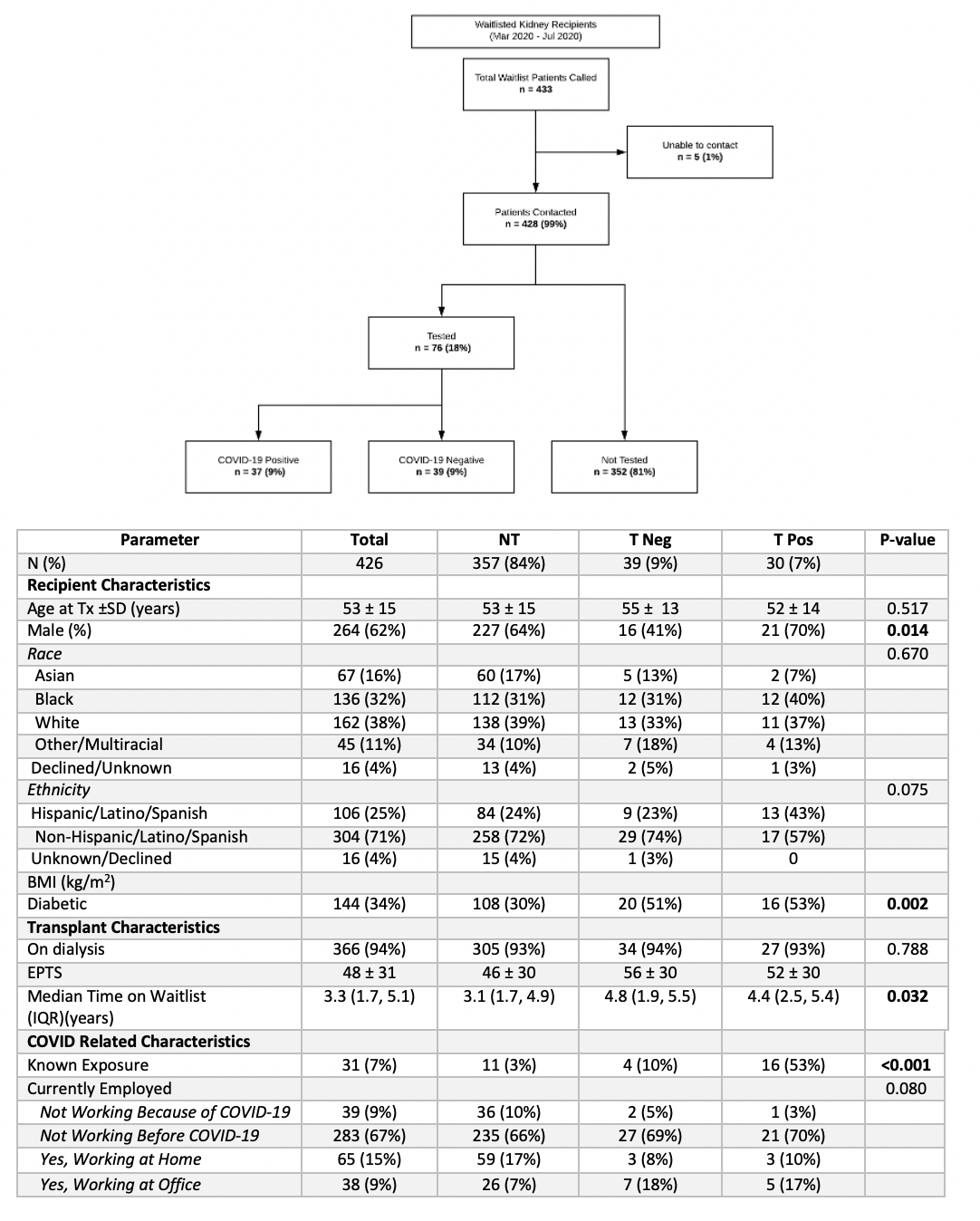
*Results: Active waitlist patients as of 4/2020 were contacted (Figure 1). Patients were stratified into 3 groups based on SARS-CoV2 testing: (1) No Test (NT) (n=357), (2) Test Neg (TNeg) (n=39), and (3) Test Pos (TPos) (n=30). Groups were similar at baseline, but differed with respect to ethnicity and diabetes status (Table 1). Black patients had a disproportionately higher rate of testing positive at 40% (n=12), even though as a group they represented 32% of our waitlist. Hispanic patients comprised 26% of the total WL patients, 43% of the COVID-19 positive patients were Hispanic. Diabetics had the highest rate of SARS CoV2 infection (p=0.02). Mortality due to COVID-19 among the WL population was 1.6% (n=7); of note, 2 additional patient deaths were reported to the center before the systematic WL calling process started. Patients who had known exposures to individuals with COVID-19 were more likely to have developed COVID-19 (p=0.001). Of the 30 TPos patients, 53% (n=16) had an exposure to a known COVID-19 infected person. This exposure was shown to be significant (p=0.001) for patients who ultimately tested positive for COVID-19. Symptoms among Tpos patients included fever (86%), body aches (68%), fatigue (64%) and cough (64%). Few patients (1%) reported changes to their social support, transportation access, and insurance coverage.
*Conclusions: During the COVID-19 pandemic solid organ transplant candidates on the WL represent a vulnerable population as a result of their end stage organ failure, and co-morbid conditions. Our systematic phone call process of WL patients identified a 7% COVID-19 incidence, 1.6% mortality rate due to COVID-19, and a low number of patients experiencing changes to their readiness for transplant. More research is needed to identify trends among the transplant WL population. It is important to uncover any geographic or socioeconomic differences across transplant centers.
To cite this abstract in AMA style:
Boyd G, Tsapepas D, Bonifacio R, Brinkers L, Brennan C, Chang A, Dalangin M, Lowe L, Mendoza JK, Mendoza JV, McNulty C, Morris M, Muttiah M, Nickason K, Ratner L. Covid-19 Impact of the Pandemic Surge on Patients Waiting for Renal Transplantation at a Single New York City Transplant Center [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/covid-19-impact-of-the-pandemic-surge-on-patients-waiting-for-renal-transplantation-at-a-single-new-york-city-transplant-center/. Accessed March 6, 2026.« Back to 2021 American Transplant Congress