Cost-Effectiveness of Transplanting Hepatitis C Donor Hearts Into Hepatitis C Uninfected Recipients
1Massachusetts General Hospital, Boston, MA, 2Brigham and Women's Hospital, Boston, MA, 3Harvard T.H. Chan School of Public Health, Boston, MA
Meeting: 2022 American Transplant Congress
Abstract number: 141
Keywords: Economics, Heart transplant patients, Hepatitis C, Waiting lists
Topic: Clinical Science » Heart » 63 - Heart and VADs: All Topics
Session Information
Session Name: Heart and VADs: All Topics I
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:40pm-5:50pm
Presentation Time: 5:40pm-5:50pm
Location: Hynes Room 210
*Purpose: To examine the clinical impact and cost-effectiveness of hepatitis C viremic (HCV+) heart organ donation in the United States.
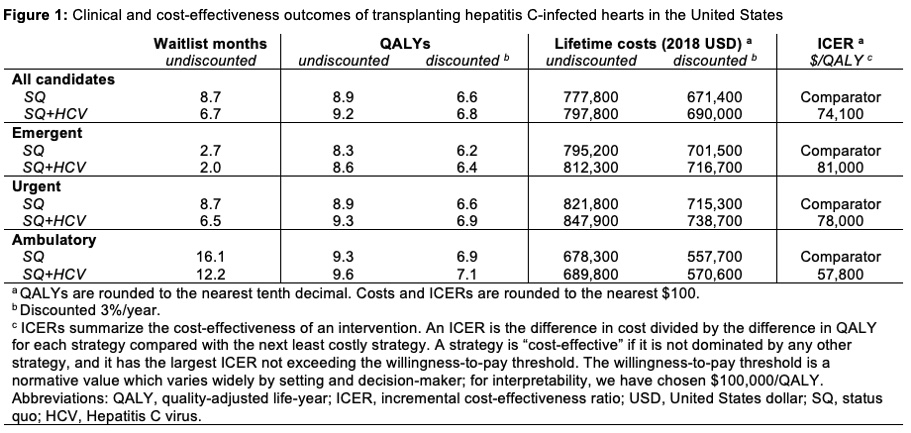
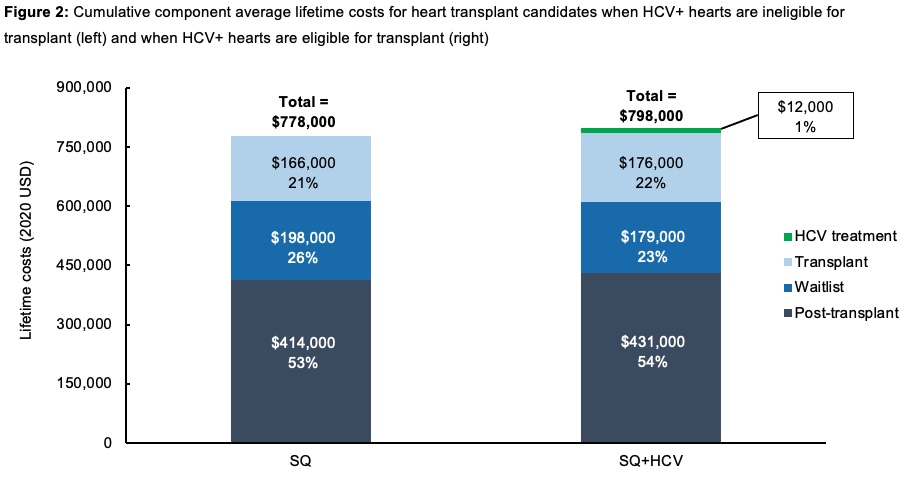
*Methods: We used a microsimulation model to compare 2 heart transplant waitlist strategies in 2018: status quo (SQ) and SQ plus HCV+ donors (SQ+HCV). We used national datasets to model mean age (53 years), male sex (75%), probabilities of waitlist mortality (0.01-0.10/month) and transplant (0.03-0.21/month) stratified by medical urgency, and post-transplant mortality (0.01-0.07/month). We assumed a 23% donor pool increase with SQ+HCV using estimates of donor HCV+ prevalence. Costs (in USD) included waitlist care ($2,200-190,000/month), transplant ($213,400), 4-week HCV treatment ($26,000), and post-transplant care ($2,500-11,300/month). We projected waitlist time, quality-adjusted life-years (QALYs), lifetime costs, and incremental cost-effectiveness ratios (ICERs [$/QALY, discounted 3%/year]; threshold ≤$100,000/QALY).
*Results: Compared to SQ, SQ+HCV decreased waitlist time (8.7 to 6.7 months), increased QALYs (8.9 to 9.2 QALYs), increased discounted lifetime costs ($671,400 to $690,000/person), and led to an ICER of $74,100/QALY (Figure 1). Urgent listing candidates had greater QALY gains vs. emergent listing candidates (0.4 vs. 0.3 QALYs) due to greater absolute decreases in waitlist time. The ICER remained ≤$100,000/QALY with ≤20% increases in transplant and post-transplant costs. HCV treatment was 1% of lifetime costs (Figure 2).
*Conclusions: Transplanting HCV+ donor hearts into uninfected recipients would decrease waitlist times, increase life expectancy, and be cost-effective. These findings were robust within the context of current HCV treatment costs.
To cite this abstract in AMA style:
Gandhi AR, Woolley AE, Baden LR, Givertz MM, Jones ML, Kim J, Mallidi HR, Mehra MR, Neilan AM. Cost-Effectiveness of Transplanting Hepatitis C Donor Hearts Into Hepatitis C Uninfected Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/cost-effectiveness-of-transplanting-hepatitis-c-donor-hearts-into-hepatitis-c-uninfected-recipients/. Accessed March 5, 2026.« Back to 2022 American Transplant Congress