Consent to Organ Offers from Public Health Service Increased Risk Donors Decreases Time to Transplant and Waitlist Mortality
Y. Kelly, A. Zarinsefat, M. Tavakol, A. Shui, C. Huang, J. P. Roberts
University of California, San Francisco, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 1598
Keywords: Donation, Ethics, HIV virus, Patient education
Topic: Clinical Science » Ethics » 23 - Non-Organ Specific: Economics & Ethics
Session Information
Session Name: Psychosocial and Treatment Adherence
Session Type: Poster Abstract
Date: Tuesday, June 7, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: The Public Health Service Increased Risk designation identified organ donors at increased risk of transmitting hepatitis B, hepatitis C, and human immunodeficiency virus. Despite clear data showing low risk of disease transmission from 0.04-4.9/10,000, many patients and families are hesitant to consent to organ offers from these donors and studies have shown these organs are highly underutilized. We hypothesize that patients who consent to offers from these donors have decreased time to transplant and decreased waitlist mortality.
*Methods: We performed a single-center retrospective review of all-comers listed for liver transplant from 2013-2019. Three competing risk events (transplant, death, and removal from transplant list) were analyzed by consent status. To control for potential confounding effects, multivariate analyses were also performed.
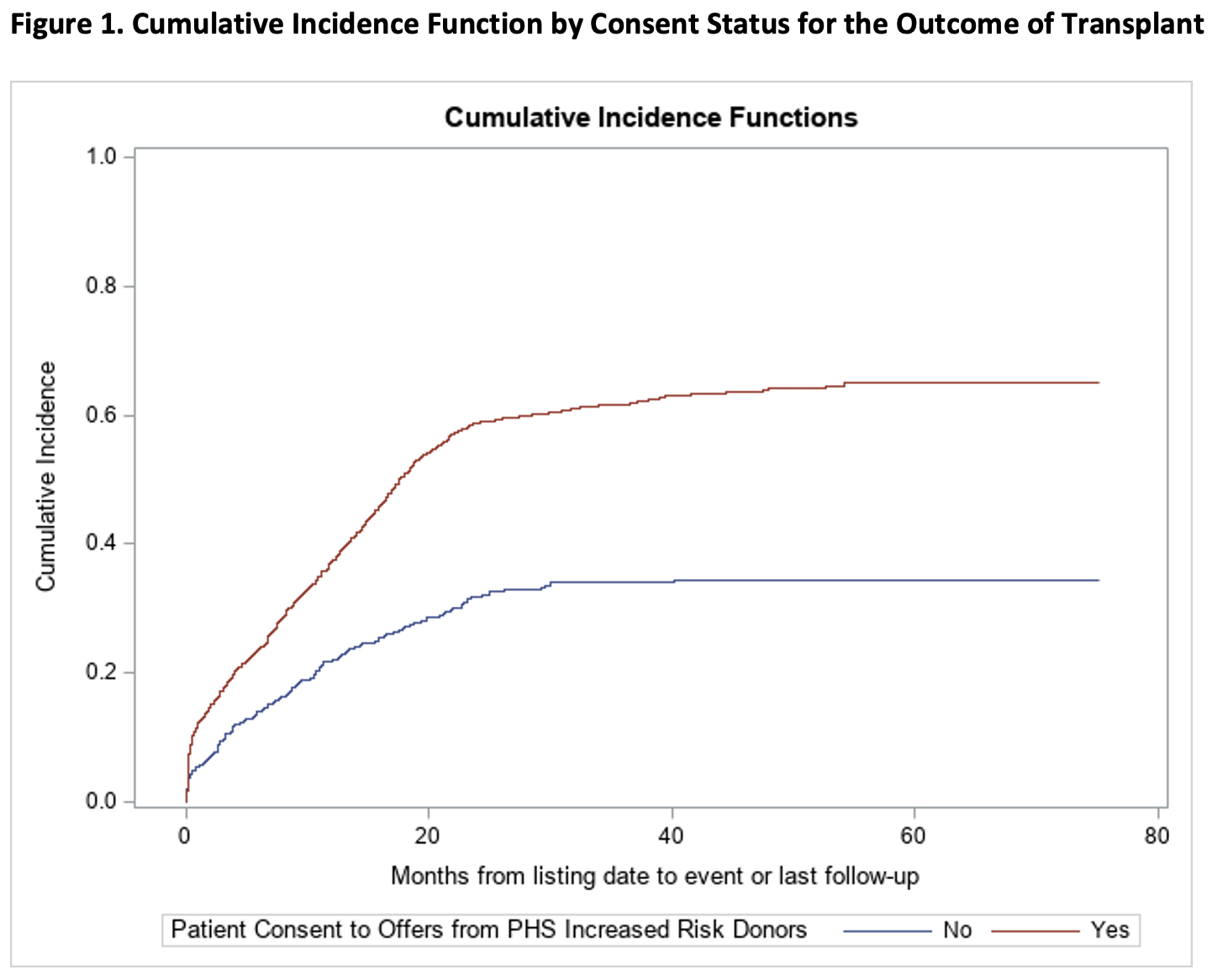
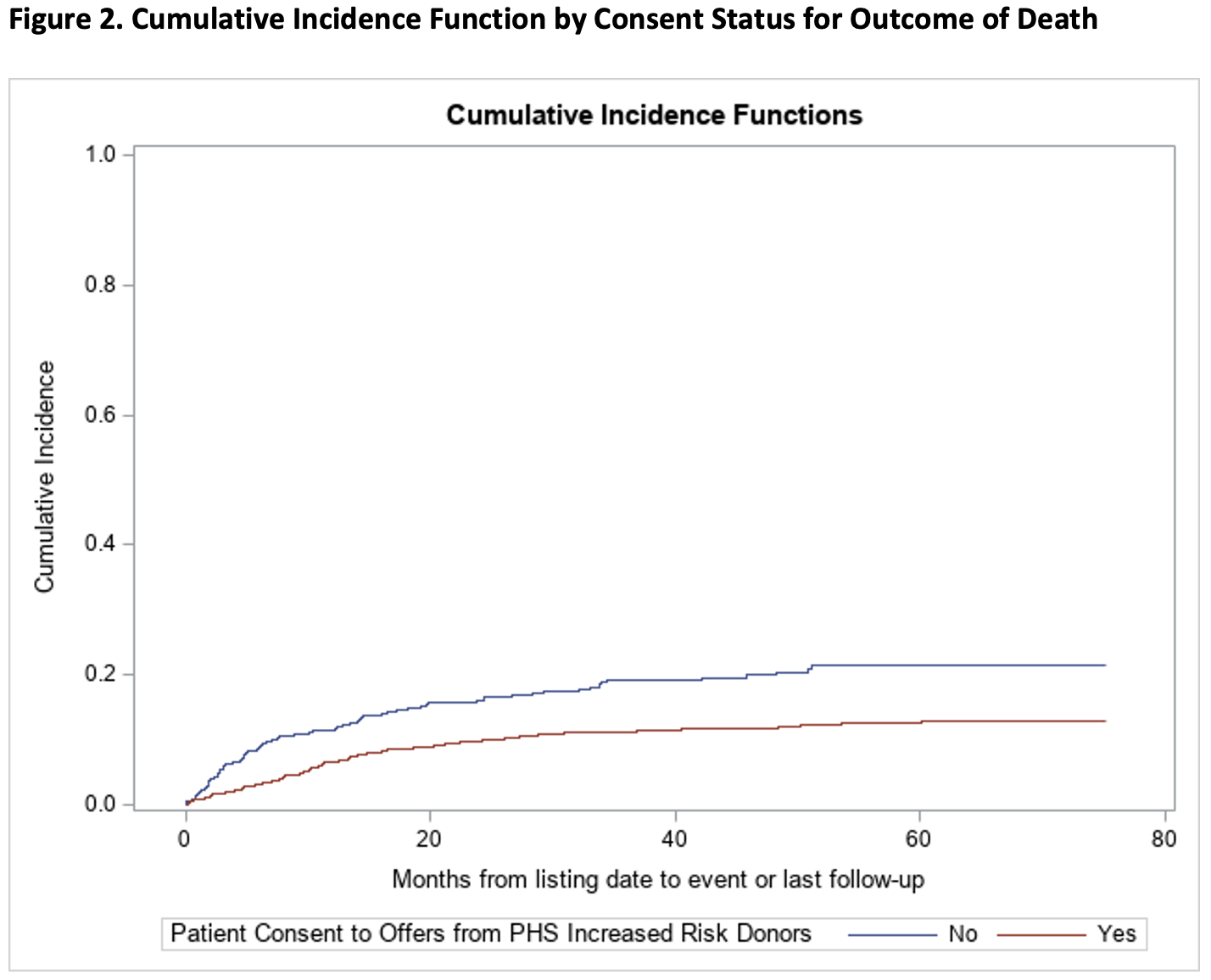
*Results: A total of 1,639 patients were included in the analysis, of which 1,276 (77.9%) consented to offers from PHS-IR donors and 363 (22.1%) did not. Compared to those who did not consent, those who did had 2.3 times the rate of transplant (SHR 2.29, 95% CI 1.88-2.79, p<0.0001), with a median time to transplant of 11 months versus 14 months (p<0.0001), and a 44% decrease in rate of death on the waitlist (SHR 0.56, 95% CI 0.42-0.74, p<0.0001). All findings remained significant after controlling for recipient age, race, gender, blood type, and MELD. Of those who did not consent, 63/359 (17.5%) received a transplant, all from standard donors, and of those who did consent, 615/1,244 (49.4%) received a transplant, of which 183/615 (29.8%) were from increased risk donors.
*Conclusions: The findings of decreased rates of transplantation and increased risk of death on the waiting list by patients who were unwilling to accept risks of viral transmission of 1/300-1/1,000 in the worst case scenarios suggests that this consent process may be harmful especially when involving “trigger” words such as HIV. The rigor of the consent process for the use of these organs was recently changed but a broader discussion about informed consent in similar situations is important.
To cite this abstract in AMA style:
Kelly Y, Zarinsefat A, Tavakol M, Shui A, Huang C, Roberts JP. Consent to Organ Offers from Public Health Service Increased Risk Donors Decreases Time to Transplant and Waitlist Mortality [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/consent-to-organ-offers-from-public-health-service-increased-risk-donors-decreases-time-to-transplant-and-waitlist-mortality/. Accessed March 3, 2026.« Back to 2022 American Transplant Congress