Comparison of Cephalexin and Ciprofloxacin Prophylaxis for Urinary Tract Infection in Kidney Transplant Recipients
N. A. Pauley, M. Fitzmaurice, A. Poparad-Stezar, B. Summers, A. Jantz
Transplant Institute, Henry Ford Hospital, Detroit, MI
Meeting: 2022 American Transplant Congress
Abstract number: 1007
Keywords: Infection, Kidney, Kidney transplantation, Prophylaxis
Topic: Clinical Science » Infection Disease » 25 - Kidney Infectious Non-Polyoma & Non-Viral Hepatitis
Session Information
Session Name: Kidney Infectious Non-Polyoma & Non-Viral Hepatitis
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Compare efficacy and safety outcomes of patients (pts) that received alternative agents as prophylaxis (ppx) for urinary tract infection (UTI) after kidney transplant (KT) as there is limited data available in those intolerant to the first-line agent sulfamethoxazole-trimethoprim (S/T).
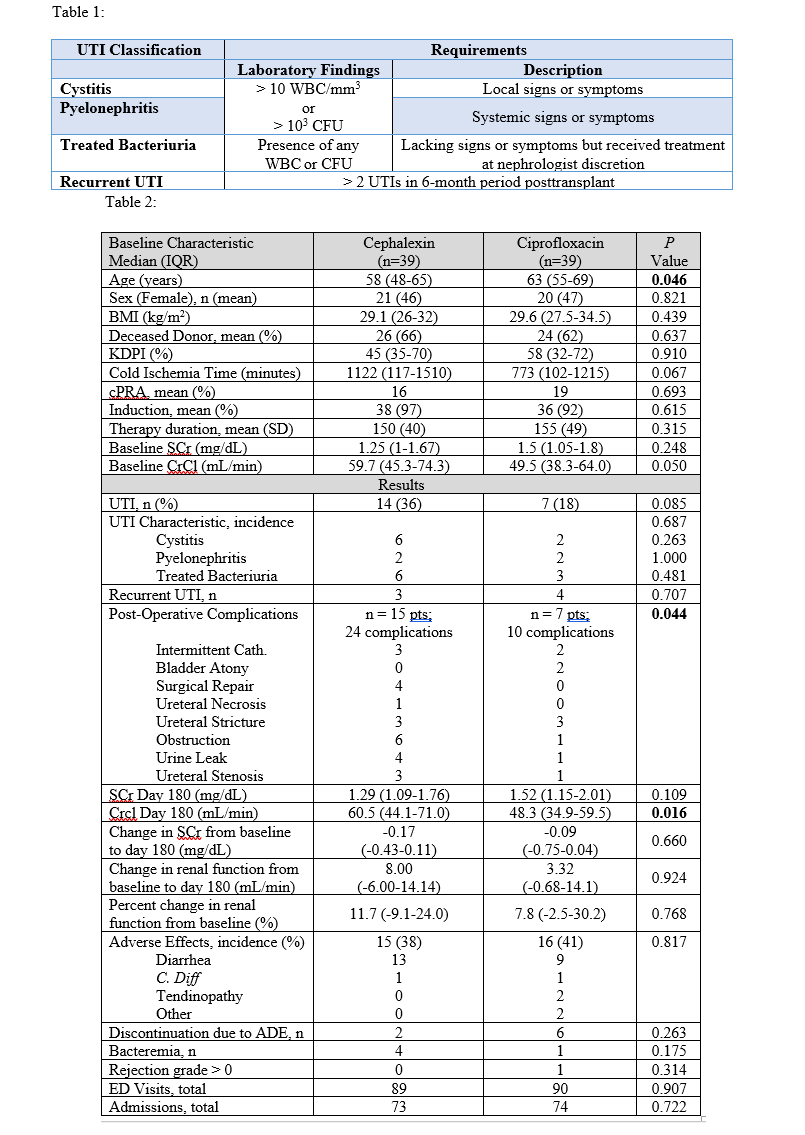
*Methods: This single-center, retrospective analysis evaluated pts who received cephalexin 500mg (CLX) or ciprofloxacin 500mg (CIP) daily for UTI ppx. Requirement for inclusion was > 30 consecutive days of therapy within 6 months post-KT in pts intolerant or allergic to S/T. The primary efficacy endpoint was ppx failure defined as clinically relevant UTI (Table 1). Secondary efficacy outcomes were UTI characteristics, change in renal function, development of resistance, and graft loss. Safety outcomes included adverse effects (ADE), discontinuations, or hospital visits.
*Results: 78 pts were included, 39 per group. Total days of therapy were 150 + 40 and 155 + 49 for CLX and CIP (p=0.315). There were no differences in baseline characteristics (See Table 2) except younger age (p=0.046) in the CLX group. Baseline creatinine clearances (CrCl; Cockcroft-Gault) were 59.7 [45.3-74.3] & 49.5 mL/min [38.3-64.0] (CLX vs CIP; p=0.05). Pts in the CLX group experienced more UTIs (CLX vs CIP: 14 (36%) vs 7 (18%); p=0.085), although the incidence did not reach statistical significance. Pts in the CLX group had more cystitis and treated bacteriuria but had significantly more post-operative complications (p=0.044). While there was a significantly lower CrCl at day 180 in the CIP group of 48.3 [34.9-59.5] vs 60.5 mL/min [44.1-71.0] (p=0.016), no difference was seen in change from baseline to day 180 (p=0.924). No significant difference was seen in the total occurrence of ADEs (p=0.817), but more pts discontinued CIP therapy (15% vs 5%; p=0.125). Development of antimicrobial resistance was similar and there was no difference in hospital visits or graft loss.
*Conclusions: Both CLX and CIP were effective at providing UTI ppx post-KT. Pts who received CLX had a higher incidence of UTIs, potentially due to more post-operative complications observed. Although CIP was discontinued more frequently, both agents were overall well tolerated while maintaining similar outcomes in renal and graft function. Overall, CLX is a suitable alternative for UTI prophylaxis in those unable to use S/T to prevent unnecessary fluoroquinolone exposure.
To cite this abstract in AMA style:
Pauley NA, Fitzmaurice M, Poparad-Stezar A, Summers B, Jantz A. Comparison of Cephalexin and Ciprofloxacin Prophylaxis for Urinary Tract Infection in Kidney Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/comparison-of-cephalexin-and-ciprofloxacin-prophylaxis-for-urinary-tract-infection-in-kidney-transplant-recipients/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress