Comparison of Cardiovascular Events by Different Types of Lipid-Lowering Drugs in Kidney Transplant Recipients
S. Bae1, J. Ahn2, M. A. Schnitzler3, K. Lentine4, D. Segev1, M. McAdams-DeMarco1
1Johns Hopkins University, Baltimore, MD, 2SOM, Johns Hopkins University, Baltimore, MD, 3Surgery, Saint Louis University, St. Louis, MO, 4Saint Louis University, St. Louis, MO
Meeting: 2022 American Transplant Congress
Abstract number: 786
Keywords: Drug interaction, Vascular disease
Topic: Clinical Science » Kidney » 35 - Kidney: Cardiovascular and Metabolic Complications
Session Information
Session Name: Kidney: Cardiovascular and Metabolic Complications
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Lipid-lowering drugs, notably statins, are one of the most widely prescribed drug classes in kidney transplant (KT) recipients. These drugs have substantially different mechanisms of action and pharmacokinetic properties. Combined with the lifelong immunosuppression and high prevalence of polypharmacy in KT recipients, these differences may render certain lipid-lowering drugs more effective than others for prevention of cardiovascular events in this population. We conducted a national study to compare the risk of cardiovascular events among commonly-used statins and non-statin lipid-lowering agents in KT recipients.
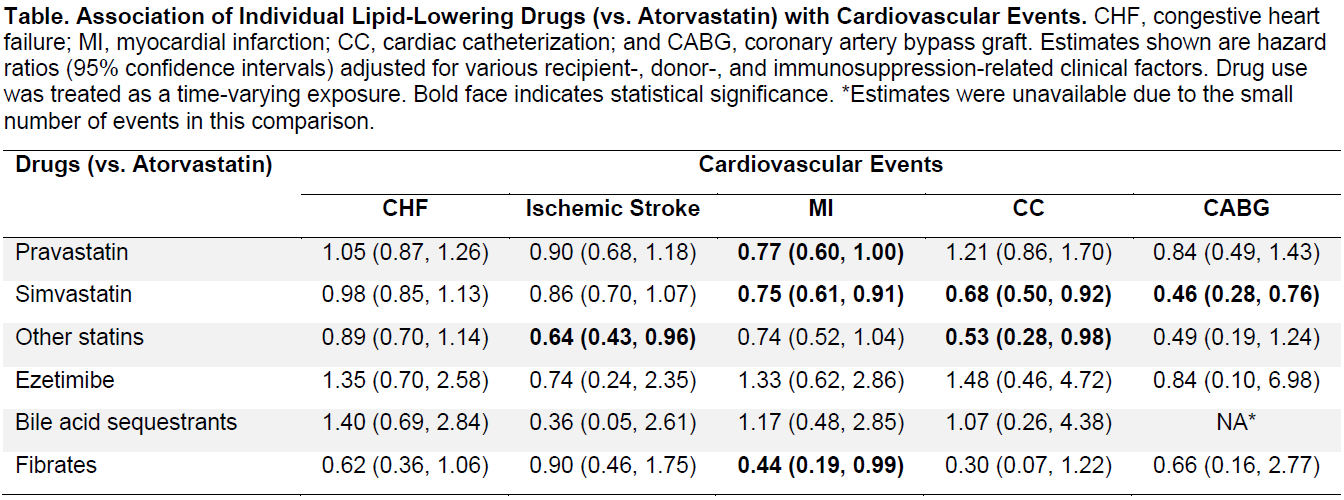
*Methods: We studied adult (≥18) single-organ KT recipients in 2006-2016 who used Medicare as primary payer (n=82,998). We used prescription drug claims to capture lipid-lowering drug use, and ICD-9/10 diagnosis codes and CPT codes to capture cardiovascular events, including congestive heart failure (CHF), ischemic stroke, myocardial infarction (MI), cardiac catheterization (CC), and coronary artery bypass graft (CABG). We conducted Cox regression for each outcome with statin use as a time-varying exposure.
*Results: Across the follow up period, 14.1% of the recipients used atorvastatin, 6.4% used pravastatin, 9.8% used simvastatin, 2.8% used other types of statins, 0.3% used ezetimibe, 1.0% used bile acid sequestrants, and 1.4% used fibrates. Compared to the atorvastatin users (Table), the hazard of ischemic stroke was significantly lower among the users of other statins (aHR=0.64 [95% CI, 0.48-0.96]), and the hazard of MI was significantly lower among the pravastatin users (aHR=0.77 [95% CI, 0.60-1.00]) and the simvastatin users (aHR=0.75 [0.61-0.91]), and the hazard of CC was lower among the simvastatin users (aHR=0.68 [0.50-0.92]) and the users of other statins (aHR=0.53 [0.28-0.98]), and the hazard of CABG was lower among the simvastatin users (aHR=0.46 [0.28-0.76]). The hazard of CHF did not significantly differ between atorvastatin and other drugs.
*Conclusions: Atorvastatin, the most commonly used lipid-lowering drugs in this population, may be less effective than others, especially simvastatin, for preventing cardiovascular events in KT recipients.
To cite this abstract in AMA style:
Bae S, Ahn J, Schnitzler MA, Lentine K, Segev D, McAdams-DeMarco M. Comparison of Cardiovascular Events by Different Types of Lipid-Lowering Drugs in Kidney Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/comparison-of-cardiovascular-events-by-different-types-of-lipid-lowering-drugs-in-kidney-transplant-recipients/. Accessed March 3, 2026.« Back to 2022 American Transplant Congress