Comparing Early Kidney after Liver Transplant (KALT) and Simultaneous Liver-Kidney Transplant (SLK): Evaluating Racial Disparities. Will Everyone Have the Same “Safety Net”?
1Wake Forest Baptist Health, Winston-Salem, NC, 2The Ohio State University Wexner Medical Center, Columbus, OH, 3Wake Forest Baptist Health, Winston-Salem, MN
Meeting: 2020 American Transplant Congress
Abstract number: LB-019
Keywords: African-American, Allocation, Kidney/liver transplantation, Survival
Session Information
Session Name: Poster Session B: Late Breaking
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: In 2017, UNOS implemented simultaneous liver-kidney transplant (SLK) guidelines that included medical eligibility criteria and a “safety net” providing prioritization on the kidney transplant (KT) waitlist for patients with early and persistent renal failure after liver transplant (LT). Given lower living donation (LD) rates among African-American (AA) patients, access to kidney after liver transplant (KALT) is an important consideration in understanding the efficacy of the “safety net”. With limited experience to evaluate racial disparities since “safety net” implementation, we compared early KALT and SLK survival in a post-MELD cohort.
*Methods: Using national UNOS data, we compared adult SLK and early KALT patients who underwent whole deceased donor (DD) LT from 2002 to 2018. Early KALT was defined as 60-365 days between LT and subsequent KT reflecting safety net listing criteria. Patient survival after LT was compared according to race including adjustment for recipient age, gender, BMI, MELD, medical condition at transplant, prior liver transplant, diabetes, renal function, and kidney donor KDPI.
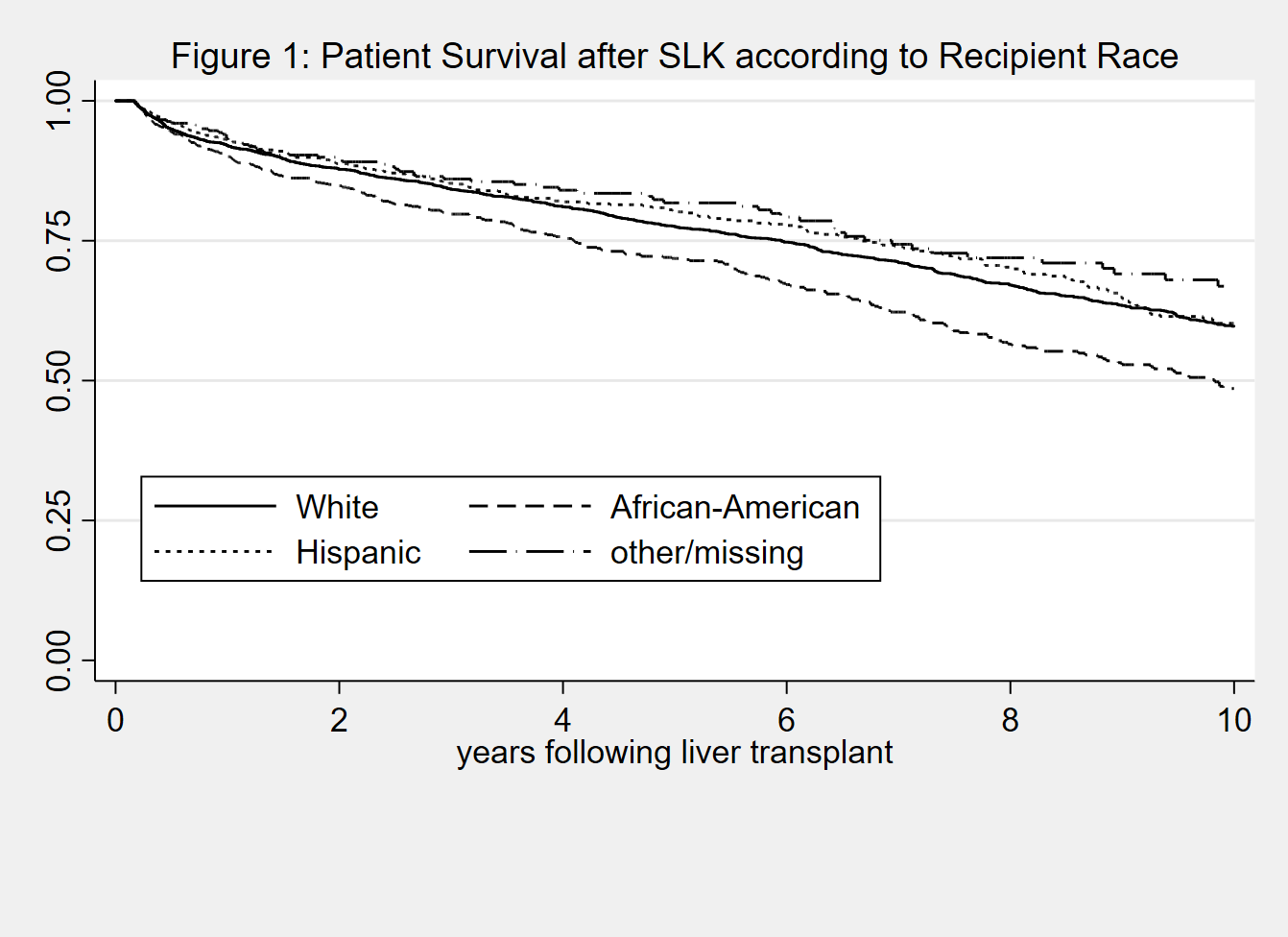
*Results: There were 6,774 SLK and 120 early KALT (77% DD). For SLK, 16% were AA recipients and 17% were Hispanic (H), but only 7% were AA and 9% H for early KALT (p<0.001). This decreased proportion remained significant even after excluding LD (DD early KALT 78% white (W), 8% AA, 11% H vs SLK 63% W, 16% AA, 17% H, p=0.002.) There were small but significant differences in KDPI of SLK donors according to recipient race (KDPI W 38±26%, AA 40±26%, H 39±26%, p=0.007). Differences were larger for DD early KALT, but not significant (KDPI W 48±22%, AA 58±22%, H 49±26%, p=0.43). There were no significant differences in survival according to recipient race for early KALT, but AA had worse unadjusted and adjusted survival after SLKT (aHR=1.23; 95%CI=1.08-1.39) (fig 1). Hispanics had improved survival after SLKT after adjusting for KDPI and recipient factors (aHR=0.86; 95%CI=0.76-0.98).
*Conclusions: During this time, there was a lower proportion of AA and H patients undergoing early KALT even after excluding LD. Higher KDPI predicted lower survival after SLK, and there were minor differences in KDPI according to recipient race for SLK and early KALT. Early KALT survival did not differ according to race, but AA patients had worse survival following SLK after adjusting for recipient factors.
To cite this abstract in AMA style:
Jay C, Stratta R, Washburn W, Rogers J, Rudnick S, Reeves-Daniel A, Heimbach J. Comparing Early Kidney after Liver Transplant (KALT) and Simultaneous Liver-Kidney Transplant (SLK): Evaluating Racial Disparities. Will Everyone Have the Same “Safety Net”? [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/comparing-early-kidney-after-liver-transplant-kalt-and-simultaneous-liver-kidney-transplant-slk-evaluating-racial-disparities-will-everyone-have-the-same-safety-net/. Accessed March 1, 2026.« Back to 2020 American Transplant Congress