Comparable Risk of End-Stage Renal Disease (ESRD) in Liver Transplant Alone (LTA) and Simultaneous Liver Kidney (SLK) Recipients Who Had Pre-LT Kidney Biopsy for Renal Dysfunction or Proteinuria
Transplantation, Mayo Clinic, Jacksonville, FL
Meeting: 2013 American Transplant Congress
Abstract number: D1685
Data concerning the utility of kidney biopsy in liver transplant (LT) candidates with renal dysfunction and/or proteinuria is lacking. Methods: 67 LT candidates with iothalamate GFR<40 ml/min and/or proteinuria underwent pre-LT percutaneous kidney biopsy. Candidates with interstitial fibrosis (IF) or glomerulosclerosis (GS) ≥30% received simultaneous liver-kidney transplantation (SLK, n=25), while the remaining patients received LT alone (LTA) (n=42). Primary endpoint was the incidence of ESRD at last post-tx follow-up (FU). Results: Indications for kidney biopsy were GFR<40 ml/min (n=17), dialysis (n=9), proteinuria and GFR <40 (n=39) and proteinuria alone (n=2). Biopsy related bleeding occurred in 8 patients (12%). Table presents characteristics and kidney biopsy findings of LTA and SLK recipients.
| LTA (n=42) | SLK (n=25) | P | |
|---|---|---|---|
| Age (yrs) | 58±14 | 59±8 | 0.5 |
| % Male gender | 71 | 80 | 0.4 |
| % HCV | 48 | 40 | 0.6 |
| % Re-LT | 19 | 36 | 0.1 |
| % Dialysis at biopsy | 14 | 16 | 0.9 |
| Pre-LT GFR (ml/min) | 28±14 | 24±8 | 0.3 |
| 24-hr urine protein (mg/d) | 69 (0-4338) | 286 (0-7020) | 0.2 |
| Kidney size (cm) | 11±2 | 11±1 | 0.7 |
| Biopsy finding | |||
| %IF | 10±5 | 26±14 | <0.0001 |
| %GS | 14±10 | 34±17 | <0.0001 |
| %ATN/normal | 69 | 0 | <0.0001 |
| %MPGN | 17 | 16 | 0.9 |
| %Diabetic Nephropathy | 7 | 32 | 0.008 |
| MELD score at LT | 23±6 | 24±6 | 0.4 |
| FU yrs | 1.9±0.2 | 1.8±0.3 | 0.9 |
| Crt at last FU* (mg/dl) | 1.5±0.6 | 1.2±0.4 | 0.02 |
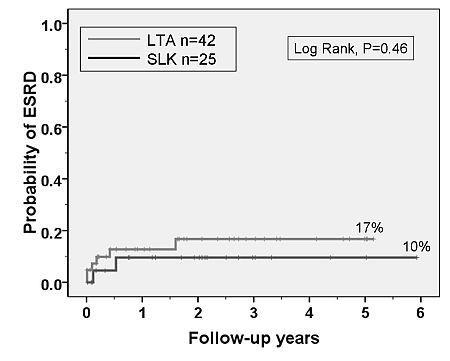
The incidence of ESRD at last FU was comparable between LTA and SLK recipients (figure).
ESRD following LTA was associated with surgical re-exploration (HR=10, CI=1.7-54, P=0.008), bacteremia (HR=9, CI=1.1-78, P=0.02) and CMV disease (HR=8.0, CI=1.5-45, P=0.01) but did not relate to dialysis at LT (P=0.2), pre-LT dialysis duration (P=0.6) or pre-LT GFR (P=0.9).
Conclusions: 1) Incidence of post-LT ESRD is comparable between LTA and SLK recipients who had pre-LT kidney biopsy for renal dysfunction and/or proteinuria. 2) Post-LT events rather than pre-LT factors determine the risk of post-LT ESRD. 3) Crt at last FU is higher but acceptable in LTA compared to SLK recipients.
To cite this abstract in AMA style:
Wadei H, Mai M, Prendergast M, Keaveny A, Pungpapong S, Gonwa T. Comparable Risk of End-Stage Renal Disease (ESRD) in Liver Transplant Alone (LTA) and Simultaneous Liver Kidney (SLK) Recipients Who Had Pre-LT Kidney Biopsy for Renal Dysfunction or Proteinuria [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/comparable-risk-of-end-stage-renal-disease-esrd-in-liver-transplant-alone-lta-and-simultaneous-liver-kidney-slk-recipients-who-had-pre-lt-kidney-biopsy-for-renal-dysfunction-or-proteinuria/. Accessed February 6, 2026.« Back to 2013 American Transplant Congress
