Chronic Kidney Disease among Liver Transplant Candidates: A Rising Burden and Its Impact on Post-Liver Transplant Outcomes
1UCSF, San Francisco, CA, 2Columbia University, New York, NY
Meeting: 2019 American Transplant Congress
Abstract number: 554
Keywords: Kidney, Kidney/liver transplantation, Liver cirrhosis
Session Information
Session Name: Concurrent Session: Liver - Kidney Issues in Liver Transplantation
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:18pm-5:30pm
Presentation Time: 5:18pm-5:30pm
Location: Room 302
*Purpose: Chronic kidney disease (CKD) is the end manifestation of persistent renal damage, a pathology distinct from the reversible acute kidney injury (AKI). This distinction is critical because a single measure of creatinine, as included within the MELD score, does not differentiate between AKI and CKD. Despite this important distinction, little is known of the burden, the determinants, and the impact of CKD among patients with cirrhosis.
*Methods: UNOS data for all patients listed for LT in the U.S. between 2002-17 were analyzed. Patients listed as status-1 or with MELD exceptions were excluded. The primary outcome was the development of CKD pre-LT: eGFR<60 ml/min for 90 days with a final eGFR of <30 ml/min OR >72 days of hemodialysis. Competing-risk analyses determined the factors associated with CKD development, accounting for LT and waitlist death. Cox-regression determined the factors associated with post-LT mortality. The proportion of the adjusted effect of pre-LT CKD on post-LT mortality that was attributable to SLKT was determined comparing coefficient estimates and confidence intervals for this effect were calculated using bias-corrected percentile bootstrap methods.
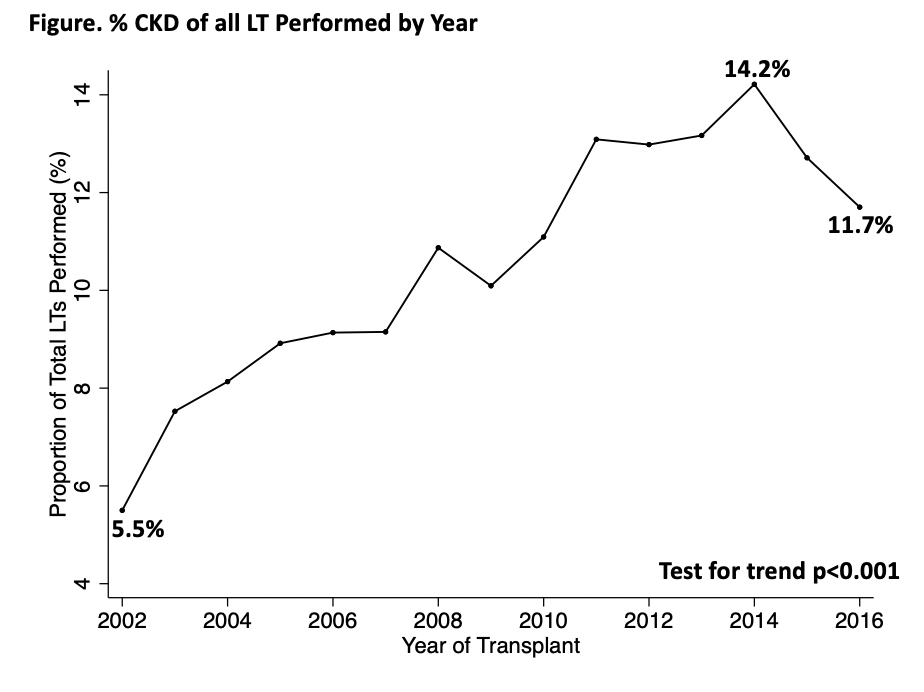
*Results: Of 68,147 LT candidates, the proportion with CKD at last follow-up increased from 5.5% in 2002 to 11.7% in 2016 (p<0.001, test for trend)(Figure). In adjusted analysis, the factors associated with the development of CKD included NASH (sHR:1.09), diabetes (sHR:1.24), age (sHR:0.98 per year), ascites (sHR:1.17), hepatic encephalopathy (sHR:1.38), MELD at listing (sHR: 0.89), and region median MELD score at LT grouping (High Median MELD Group vs. Low: sHR:1.50). Among the 36,203 patients who underwent LT, pre-LT CKD was significantly associated with post-LT mortality (HR 1.16, 95CI 1.07 – 1.25, p<0.001) even after adjusting for donor risk index, age, final MELD, etiology of cirrhosis, presence of hepatic encephalopathy, receiving a SLKT, and presence of diabetes. There was no significant mediating influence of SLKT on the effect of pre-LT CKD on post-LT survival: 1-year proportion of the attributable effect of SLKT was 10.9% (bias corrected 95CI -30.3 - 70%); 5-year proportion of the attributable effect of SLKT was 22.2% (bias corrected -12.6 - 138.2%).
*Conclusions: The rising burden of pre-LT CKD is significantly associated with increasing co-morbidities (e.g., NASH, Diabetes, Age, ascites, hepatic encephalopathy) and longer waiting time (e.g., region risk, MELD at Listing). Pre-LT CKD has a significant deleterious impact on post-LT outcomes – an impact that cannot be corrected by receiving a SLKT. These findings highlight the need for the earlier identification of CKD where the implementation of preventative measures may optimize post-liver transplant outcomes.
To cite this abstract in AMA style:
Cullaro G, Verna EC, Lee BP, Lai JC. Chronic Kidney Disease among Liver Transplant Candidates: A Rising Burden and Its Impact on Post-Liver Transplant Outcomes [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/chronic-kidney-disease-among-liver-transplant-candidates-a-rising-burden-and-its-impact-on-post-liver-transplant-outcomes/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress