Changes in Body Composition One Year after Hand-Assisted Laparoscopic Donor Nephrectomy in Living Kidney Donors
H. Fukuhara1, Y. Watarai1, S. Narumi1, N. Goto1, T. Hiramitsu1, M. Okada1, K. Futamura1, T. Tomosugi1, A. Kanda1, T. Nawano1, N. Tsuchiya2
1Department of Transplant Nephrology and Surgery, Nagoya Daini Red Cross Hospital, Myoukentyou, Japan, 2Department of Urology, Yamagata University Faculty of Medicine, Yamagata City, Iidanishi, Japan
Meeting: 2020 American Transplant Congress
Abstract number: A-031
Keywords: Donors, unrelated, Kidney transplantation, N/A
Session Information
Session Name: Poster Session A: Kidney Living Donor: Other
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The aim of this study was to investigate the effect of surgery on living donors’ body composition and to clarify the factors related to the body composition changes.
*Methods: Based on preoperative computed tomography (CT) images of 335 living kidney donors (127 male, 209 female), we evaluated the following three body composition parameters to calculate body composition changes with aging by gender using simple linear regression: 1) skeletal muscle mass, which were quantified by the skeletal muscle index (SMI) and calculated using the skeletal muscle area from an L3 level CT, 2) fat distribution, which were calculated the visceral adipose tissue (VAT)/subcutaneous adipose tissue (SAT) ratio using the intra and extra peritoneal fat area, respectively from an umbilical-level CT, and 3) muscle quality, which were quantified by the intramuscular adipose tissue content (IMAC) and determined using an L3 level CT; this was calculated using the mean CT value of the region of interest (ROI) of the multifidus muscle (Hounsfield unit: HU)/the mean CT value of the ROI of the subcutaneous fat (HU).Thereafter, with the pre- and postoperative CT images from 75 living kidney donors (25 male, 50 female) who had undergone hand-assisted laparoscopic donor nephrectomy (HALDN), we compared the pre- and postoperative changes in body composition.
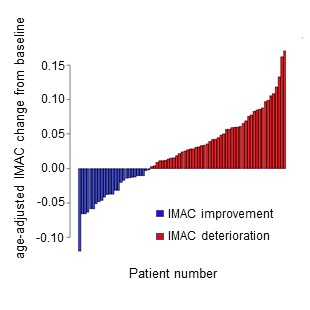
*Results: The annual change in the IMAC with age was 0.0049 in men and 0.0091 in women. Of the 75 patients, 49 (65.3%; 16 male, 33 female) had worse muscle quality (Figure), and the IMAC was significantly higher after the nephrectomy (p < 0.001). In these 49 patients, the median (range) change in IMAC was 0.061 (0.018-0.11) in men, and 0.052 (0.017-0.18) in women. Univariate analysis revealed that the SMI and VAT/SAT ratio changes were significantly different between the IMAC improvement and deterioration groups. On multivariate analysis, the SMI change was identified as an independent factor for the IMAC change (odds ratio 1.12, p = 0.0019). The IMAC change was negatively correlated with the SMI change (r = -0.40).
*Conclusions: Although muscle quality worsens after HALDN, maintaining muscle mass is a significant factor to retain muscle quality. To maintain the donor’s health, a muscle rehabilitation program including an exercise regime should be recommended to donors after the nephrectomy.
To cite this abstract in AMA style:
Fukuhara H, Watarai Y, Narumi S, Goto N, Hiramitsu T, Okada M, Futamura K, Tomosugi T, Kanda A, Nawano T, Tsuchiya N. Changes in Body Composition One Year after Hand-Assisted Laparoscopic Donor Nephrectomy in Living Kidney Donors [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/changes-in-body-composition-one-year-after-hand-assisted-laparoscopic-donor-nephrectomy-in-living-kidney-donors/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress