Change in Hypertension (HTN) Guidelines in Living Kidney Donors (LKDs) and Long-Term Renal Outcomes
1Mayo Clinic Rochester, Rochester, MN, 2Mayo Clinic Rochester, Scottsdale, AZ
Meeting: 2020 American Transplant Congress
Abstract number: C-080
Keywords: Donation, Proteinuria, Renal dysfunction
Session Information
Session Name: Poster Session C: Kidney Living Donor: Long Term Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: There is limited knowledge regarding the long-term renal outcomes in hypertensive LKDs. We performed a multicenter study assessing long-term outcomes with or without HTN at the time of donation using emerging definitions with both office and ambulatory BP (ABP) readings.
*Methods: We prospectively followed LKDs from 1999 to 2012. We studied all donors who completed the survey or had clinical follow-up between 2017 and 2019. Different definitions of HTN were assessed: h/o of HTN (HxHTN) was defined as a kidney donor with a diagnosis of HTN prior to donor evaluation; antihypertensive medications use (antiHTN meds). Office HTN was defined as having HxHTN or taking antiHTN meds or having office BP ≥ 140/90 (JNC7) or ≥ 130/80 (ACC/AHA 2017). Ambulatory Blood Pressure Monitoring (ABPM) HTN was defined as having HxHTN or taking antiHTN meds or an Active (daytime) ABPM > 135/85 (JNC7) or > 130/80 (ACC/AHA 2017). A non-dipper was defined as the ratio of mean nocturnal and active ABPM greater than 90% for systolic or diastolic readings. Renal outcomes were eGFR<45, 40% decline in eGFR, or proteinuria. Logistic regression was used for analysis, unadjusted and adjusted for age, sex, follow-up time.
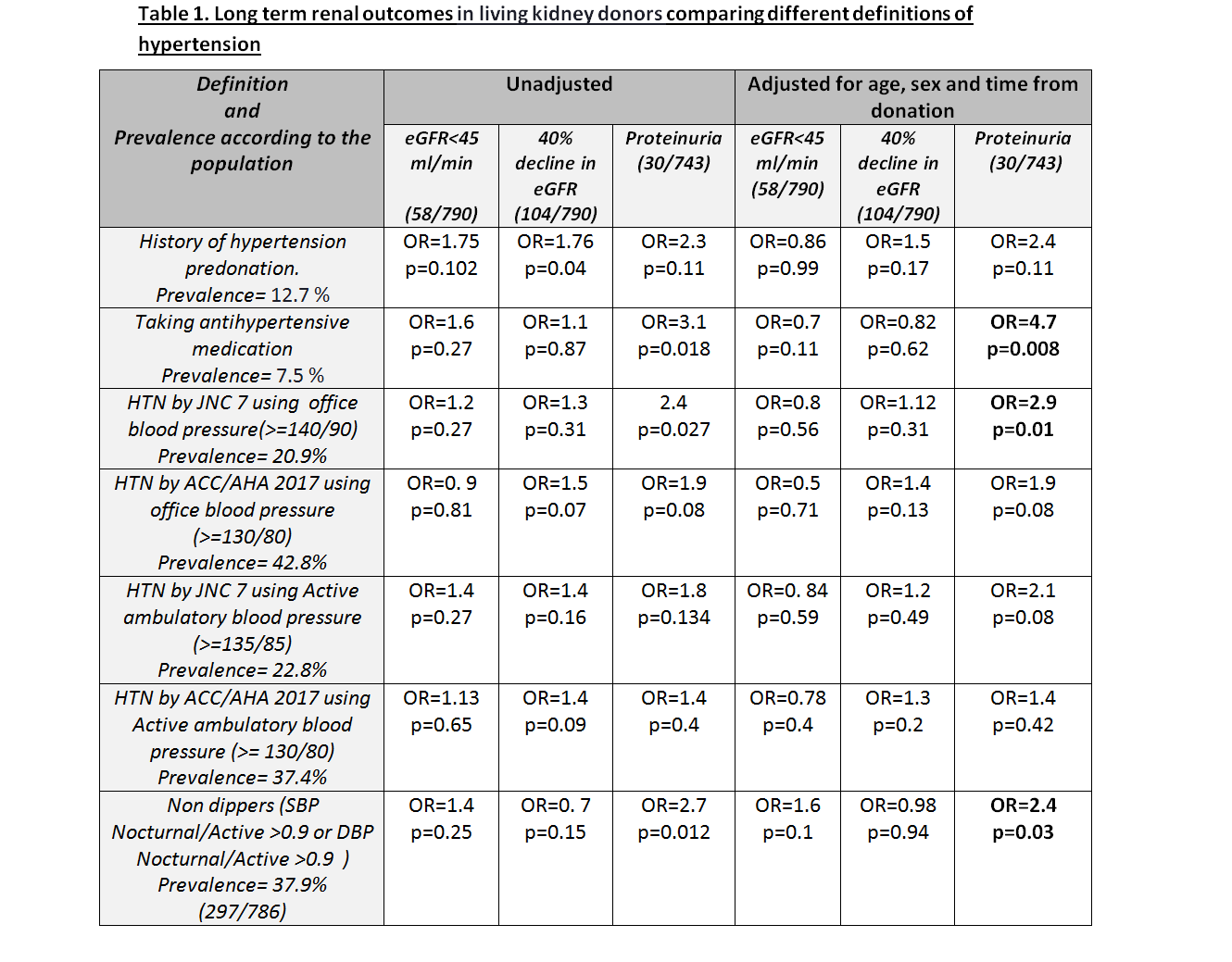
*Results: A total of 918 kidney donors who had ABPM were analyzed with a mean 10.6 years of follow-up. As seen in Table 1, none of the HTN definitions and types of measurements were predictor for eGFR<45 ml/min or a 40% decline in eGFR. History of taking antiHTN meds and office HTN by JNC7 predicted proteinuria in the adjusted model. Nondipper status also predicted proteinuria (OR=2.4, p=0.034).
*Conclusions: We did not detect a long-term risk for clinically significant reductions in GFR among hypertensive donors using different definitions of HTN. However, given the increased risk for proteinuria among hypertensive LKDs, longer follow-up is needed to determine its potential clinical impact.
To cite this abstract in AMA style:
Merzkani M, Denic A, D'Costa M, Ricaurte L, Narasimhan R, Benavides X, Mullan A, Larson J, Kremer W, Park W, Alexander MP, Chakkera H, Textor S, Taler S, Stegall M, Issa N, Rule A. Change in Hypertension (HTN) Guidelines in Living Kidney Donors (LKDs) and Long-Term Renal Outcomes [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/change-in-hypertension-htn-guidelines-in-living-kidney-donors-lkds-and-long-term-renal-outcomes/. Accessed March 12, 2026.« Back to 2020 American Transplant Congress