Associations Between Provision of Transplant Pharmacy Services and Center-Level Patient and Graft Outcomes in U.S. Adult Kidney Transplant Programs.
1Univ of Michigan, Ann Arbor
2Univ of Pennsylvania, Philadelphia
3Univ of Cincinnati, Cincinnati
4Medical Univ of South Carolina, Charleston
Meeting: 2017 American Transplant Congress
Abstract number: A271
Keywords: Kidney transplantation, Outcome
Session Information
Session Name: Poster Session A: Transplant Economics and Pharmacy Value Initiatives
Session Type: Poster Session
Date: Saturday, April 29, 2017
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall D1
As a follow up to a U.S. transplant pharmacist workforce survey in 2013-14 (AJT 2015;15:2683-90), we assessed associations between transplant pharmacist involvement and daily activities with center-level patient and graft outcomes for adult renal transplant recipients. In a cross-sectional study, pharmacist survey responses were linked with center-specific outcomes data from the Scientific Registry of Transplant Recipients (100 of 190 centers) and the University HealthSystem Consortium (61 of 94 centers). Centers responding to the survey (RS-centers) performed more transplants than non-responding centers (NRS-centers). First-year patient or graft survival was not associated with particular pharmacist staffing level and training, patient care activities or pharmacy department operations. Transplant pharmacists at the centers in the bottom quartile for 1-year patient or graft survival were more likely to participate in medication dispensing compared to the centers with the better outcomes, but the difference did not reach statistical significance (33% vs. 17%, p=0.066). More centers in the upper 3 quartiles had a transplant pharmacist participating in transplant selection committee compared to the centers in the bottom quartile, but the difference was not significant (39% vs. 25%, p=0.154). 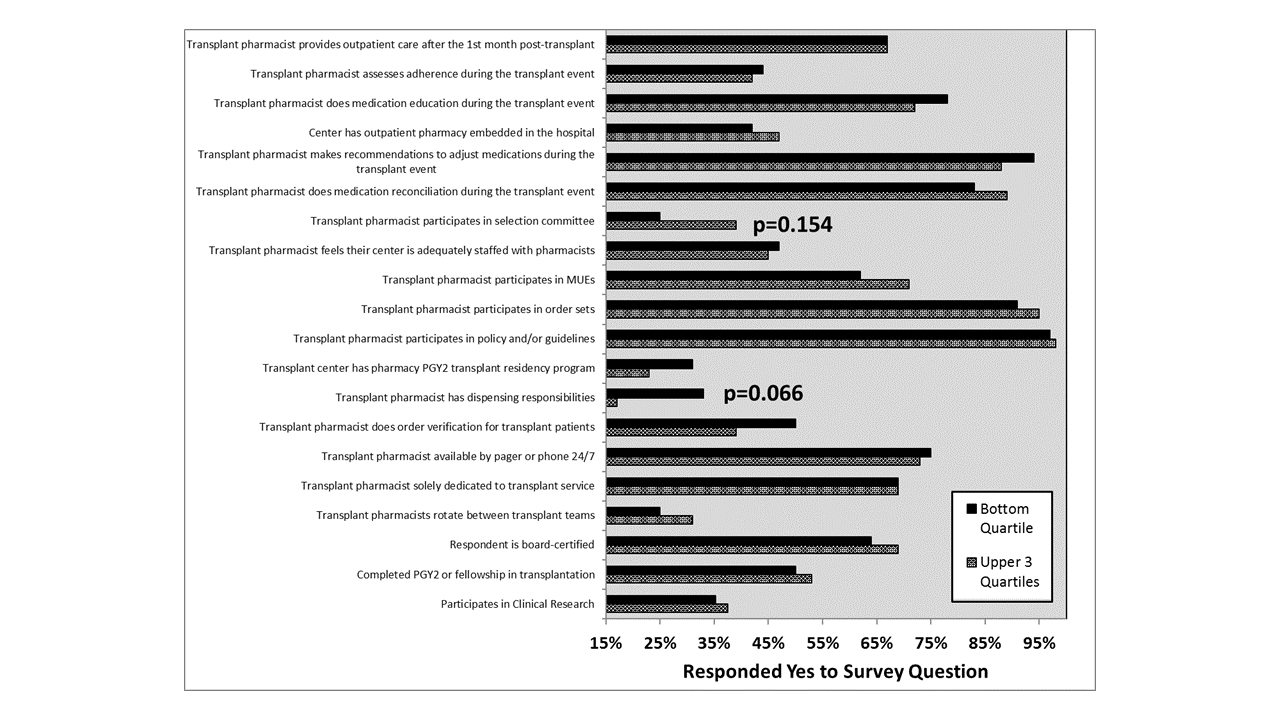 Lower Clostridium difficile enteritis rates (-7.0 cases per 1,000 transplant events, 95% CI -13.3 to -0.7, p=0.030) were observed during the transplant surgical events in RS-centers vs. NRS-centers. Shorter length of stay was observed in centers where a pharmacist participated in clinical research (5.7 ± 1.2 vs. 6.8 ± 1.8 days, p=0.014) and that had a PGY2 transplant pharmacy program (6.0 ± 1.5 vs. 7.6 ± 1.6 days, p<0.001). These associations may suggest structural advantages that enable better processes of care to improve clinical outcomes in high-volume centers. However, further evaluation of a transplant pharmacist's impact on objective parameters under current practice models is needed.
Lower Clostridium difficile enteritis rates (-7.0 cases per 1,000 transplant events, 95% CI -13.3 to -0.7, p=0.030) were observed during the transplant surgical events in RS-centers vs. NRS-centers. Shorter length of stay was observed in centers where a pharmacist participated in clinical research (5.7 ± 1.2 vs. 6.8 ± 1.8 days, p=0.014) and that had a PGY2 transplant pharmacy program (6.0 ± 1.5 vs. 7.6 ± 1.6 days, p<0.001). These associations may suggest structural advantages that enable better processes of care to improve clinical outcomes in high-volume centers. However, further evaluation of a transplant pharmacist's impact on objective parameters under current practice models is needed.
CITATION INFORMATION: Park J, Trofe-Clark J, Kaiser T, Pilch N, Taber D. Associations Between Provision of Transplant Pharmacy Services and Center-Level Patient and Graft Outcomes in U.S. Adult Kidney Transplant Programs. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Park J, Trofe-Clark J, Kaiser T, Pilch N, Taber D. Associations Between Provision of Transplant Pharmacy Services and Center-Level Patient and Graft Outcomes in U.S. Adult Kidney Transplant Programs. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/associations-between-provision-of-transplant-pharmacy-services-and-center-level-patient-and-graft-outcomes-in-u-s-adult-kidney-transplant-programs/. Accessed February 26, 2026.« Back to 2017 American Transplant Congress
