Association of Immunosuppressive Therapy Regimen with Sepsis Outcomes among Kidney Transplant Recipients
1University of Alabama at Birmingham, Birmingham, AL
2University of Michigan, Ann Arbor, MI
3University of Texas Health Science Center, Houston, TX.
Meeting: 2018 American Transplant Congress
Abstract number: D163
Keywords: Bacterial infection, Immunosuppression, Kidney transplantation, Outcome
Session Information
Session Name: Poster Session D: Kidney Infectious
Session Type: Poster Session
Date: Tuesday, June 5, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
OBJECTIVE: Immunosuppressive therapy (IST) could impact sepsis outcomes by altering the host immune response. We examined the associations of IST regimens with sepsis outcomes among kidney transplant recipients (KTRs).
METHODS: We conducted a retrospective cohort study using data from the United States Renal Data System. The study population included adult primary KTRs receiving transplants between 2004 and 2013 whose graft survived six months. IST regimens included: anti-thymocyte globulin (ATG)-tacrolimus (Tac)-mycophenolic acid or azathioprine (MPA/AZA)-corticosteroid (CS) [reference regimen], ATG-Tac-MPA/AZA, basiliximab/daclizumab-Tac-MPA/AZA-CS, alemtuzumab-Tac-MPA/AZA, no induction-Tac-MPA/AZA-CS, sirolimus, or cyclosporine. Sepsis events were identified based on discharge diagnoses. We used Cox models to calculate hazard ratios (HRs) with 95% confidence intervals (CIs) for 90-day mortality and Poisson models to calculate risk ratios (RRs) for in-hospital mortality.
RESULTS: A total of 68,026 KTRs met inclusion criteria and there were 5,165 sepsis events. Among those hospitalized for sepsis, the reference regimen was most common (49.4%). Overall, 90-day mortality was 60.9 per 100 person-years (py) and in-hospital mortality was 9.5%. Mortality within 90 days was lowest for the reference regimen (52.1 per 100 py) but highest for alemtuzumab-Tac-MPA/AZA (71.1 per 100 py) and sirolimus (78.9 per 100 py). In-hospital mortality was higher for alemtuzumab-Tac-MPA/AZA (11.6%) and sirolimus (13.1%) versus the reference regimen (8.4%). After adjustment for recipient factors, the alemtuzumab-Tac-MPA/AZA regimen was associated with higher 90-day and in-hospital mortality. Adjusted risks of mortality were also higher for sirolimus and lower for cyclosporine.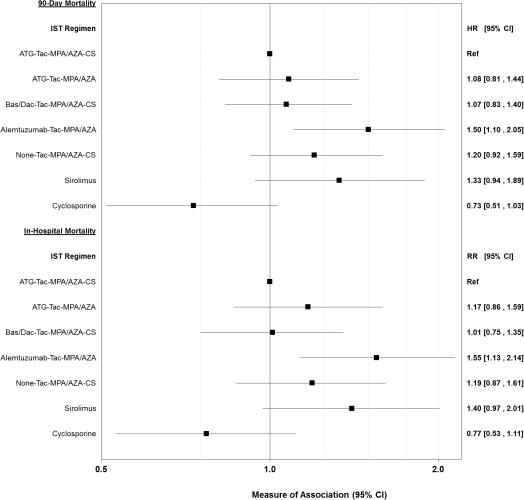
CONCLUSIONS: Alemtuzumab- and sirolimus-based regimens were associated with higher mortality among KTRs hospitalized for sepsis. These populations of recipients could benefit from efforts to improve sepsis outcomes.
CITATION INFORMATION: Donnelly J., MacLennan P., Mannon R., Saran R., Baddley J., Wang H., McGwin, Jr. G., Muntner P. Association of Immunosuppressive Therapy Regimen with Sepsis Outcomes among Kidney Transplant Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Donnelly J, MacLennan P, Mannon R, Saran R, Baddley J, Wang H, McGwin G, Muntner P. Association of Immunosuppressive Therapy Regimen with Sepsis Outcomes among Kidney Transplant Recipients [abstract]. https://atcmeetingabstracts.com/abstract/association-of-immunosuppressive-therapy-regimen-with-sepsis-outcomes-among-kidney-transplant-recipients/. Accessed February 19, 2026.« Back to 2018 American Transplant Congress
