Association of Dialysis Facility Neighborhood Socioeconomic Status with Barriers to Kidney Transplant.
1Department of Epidemiology, Rollins School of Public Health, Atlanta
2Department of Surgery, Emory University School of Medicine, Atlanta
3Department of Behavioral Sciences and Health Education, Rollins School of Public Health, Atlanta
4Department of Medicine, Columbia University Medical Center, New York
Meeting: 2017 American Transplant Congress
Abstract number: C44
Keywords: Kidney transplantation
Session Information
Session Name: Poster Session C: Disparity in Access and Outcomes for Solid Organ Transplantation
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Introduction: Dialysis facilities in neighborhoods with low socioeconomic status (SES) have lower facility-level transplantation rates. We estimated the association between barriers to transplantation and facility-area SES. Methods: Medical directors and nurse managers at United States (US) dialysis facilities in the lowest tertile of waitlisting were surveyed (N=1,527). Respondents were asked about barriers to transplant and were included in this analysis if they provided a valid zip code (N=656). Facilities were matched to the Area Deprivation Index (ADI), a composite measure of neighborhood SES that includes education, income, and housing characteristics; high ADI indicates low SES. Chi-square analyses were used to test the association between ADI (in quartiles) and facility-reported barriers to transplant. Results: Barriers to transplant frequently identified by survey respondents included patient ineligibility (75.8%), patient financial barriers (60.2%), lack of patient interest (57.8%), and distance between facility and transplant center (37.4%). ADI was significantly associated with facility-reported lack of patient interest (p=0.016) and distance barriers (p<0.001); this association increased in magnitude as ADI increased. 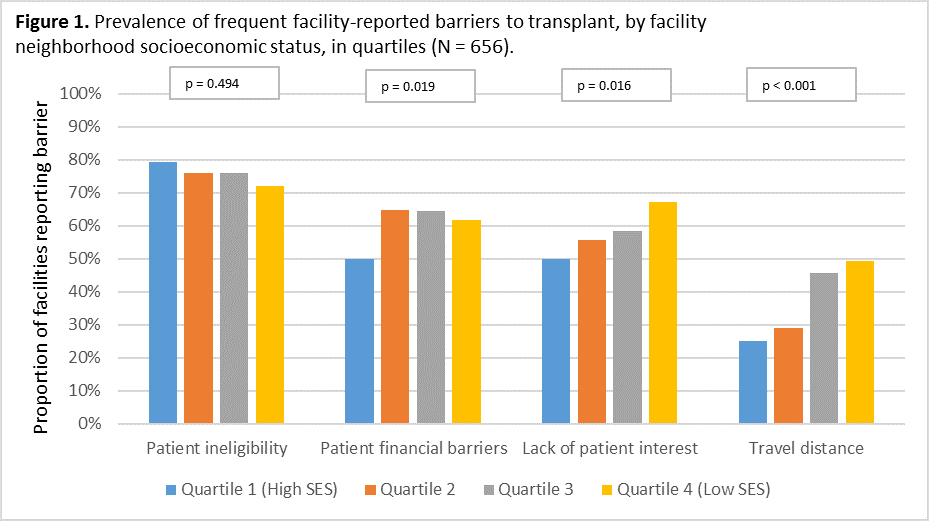 ADI was significantly associated with facility-reported patient financial barriers (p=0.019), but did not display a dose response pattern. Conclusions: Lower dialysis facility neighborhood SES was associated with greater likelihood of facility-reported structural barriers to transplant (distance, financial barriers) and lack of patient interest in a sample of US dialysis facilities with low waitlisting. Interventions targeted at facilities in low-SES neighborhoods that address these barriers could improve transplant access in these facilities.
ADI was significantly associated with facility-reported patient financial barriers (p=0.019), but did not display a dose response pattern. Conclusions: Lower dialysis facility neighborhood SES was associated with greater likelihood of facility-reported structural barriers to transplant (distance, financial barriers) and lack of patient interest in a sample of US dialysis facilities with low waitlisting. Interventions targeted at facilities in low-SES neighborhoods that address these barriers could improve transplant access in these facilities.
CITATION INFORMATION: Ross K, Basu M, Escoffery C, Gander J, Mohan S, Pastan S, Plantinga L, Smith K, Patzer R. Association of Dialysis Facility Neighborhood Socioeconomic Status with Barriers to Kidney Transplant. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ross K, Basu M, Escoffery C, Gander J, Mohan S, Pastan S, Plantinga L, Smith K, Patzer R. Association of Dialysis Facility Neighborhood Socioeconomic Status with Barriers to Kidney Transplant. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/association-of-dialysis-facility-neighborhood-socioeconomic-status-with-barriers-to-kidney-transplant/. Accessed February 20, 2026.« Back to 2017 American Transplant Congress
