Assessment of Deceased Donor Kidney and Liver Surgical Recovery Error Rates
Gift of Life Donor Program, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: 33
Keywords: Kidney/liver transplantation, Quality of life, Surgical complications
Session Information
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: There is no nationally available data related to the incidence of surgical errors in deceased donor organ recoveries or its impact on organ discard rates. Establishing effective data collection and reporting procedures regarding surgical errors made during organ recoveries is essential to OPO quality assurance programs.
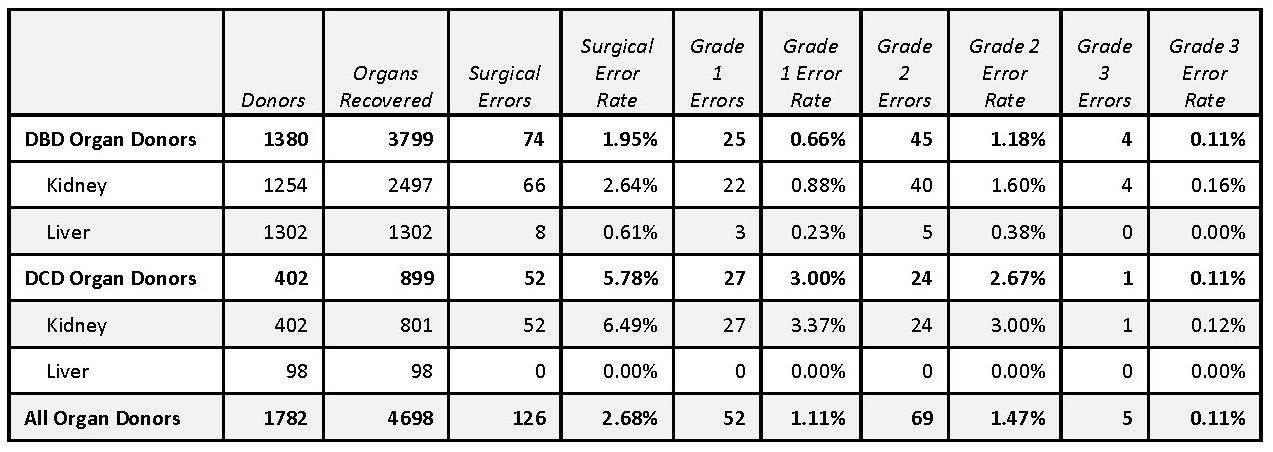
*Methods: This was a single OPO, multi-center study. The OPO collected information from the transplanting surgeon on every local organ intended for transplant. Photographs of the presumed damage were requested. Reported errors were categorized as minor (Grade 1) when the usability of the organ was not greatly altered but were technical flaws, moderate (Grade 2) when transplantability was jeopardized or significant reconstruction effort was required by the transplanting surgeon or major (Grade 3) when the dominant reason an organ was not transplanted. Surgical error rates were calculated by dividing the number of surgical errors by the number of organs recovered. The OPO Medical Director reviewed all error reports and assisted the OPO in the classification of each error. Recovery errors were communicated to the recovery surgeons in addition to being reported to and reviewed by the OPO’s Medical Advisory and Policy Board.
*Results: Over 35 months from 1/1/2017 to 11/30/2019, 153 surgeons (58 local, 95 out-of-town) recovered 3,298 kidneys and 1,400 livers for transplant. There were 126 surgical errors identified including 52 Grade 1, 69 Grade 2 and 5 Grade 3 errors resulting in an overall surgical error rate of 2.11%. Photographs were provided in 95 (75%) cases. The reported surgical error rate was significantly higher for kidneys than livers (3.58% vs. 0.57%; p < 0.0001). The DCD kidney surgical error rate was significantly higher than the DBD kidney surgical error rate (6.49% vs. 2.64%; p < 0.0001). There was no significant difference in surgical error rates between local and out-of-town surgeons (2.69% vs. 2.62%; p=1.000). Surgical error was identified as the dominant reason for organ discard in 7 (0.11%) cases.
*Conclusions: OPOs should measure surgical error rates to provide feedback to recovery surgeons. Protocols to minimize DCD kidney recovery errors should be developed.
To cite this abstract in AMA style:
Hasz RD, West SM, Nathan HM. Assessment of Deceased Donor Kidney and Liver Surgical Recovery Error Rates [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/assessment-of-deceased-donor-kidney-and-liver-surgical-recovery-error-rates/. Accessed February 25, 2026.« Back to 2020 American Transplant Congress