Assessment and Validation of Potential Predictors of Non-Adherence in Contemporary Kidney Transplant Recipients
T. Harrison, C. Perez, N. Patel, H. Meadows, J. Fleming, N. Pilch, B. O'Brien, H. Corbo, J. Hardcopf, P. Baliga, D. DuBay, D. Taber.
Medical University of South Carolina, Charleston, SC.
Meeting: 2018 American Transplant Congress
Abstract number: 128
Keywords: High-risk, Kidney transplantation, Risk factors
Session Information
Session Name: Concurrent Session: Kidney Psychosocial - 1
Session Type: Concurrent Session
Date: Sunday, June 3, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:18pm-5:30pm
Presentation Time: 5:18pm-5:30pm
Location: Room 210
The aim of this study is to assess the associations between traditional proxies of medication non-adherence and graft outcomes in contemporary kidney transplant recipients (KTRs).
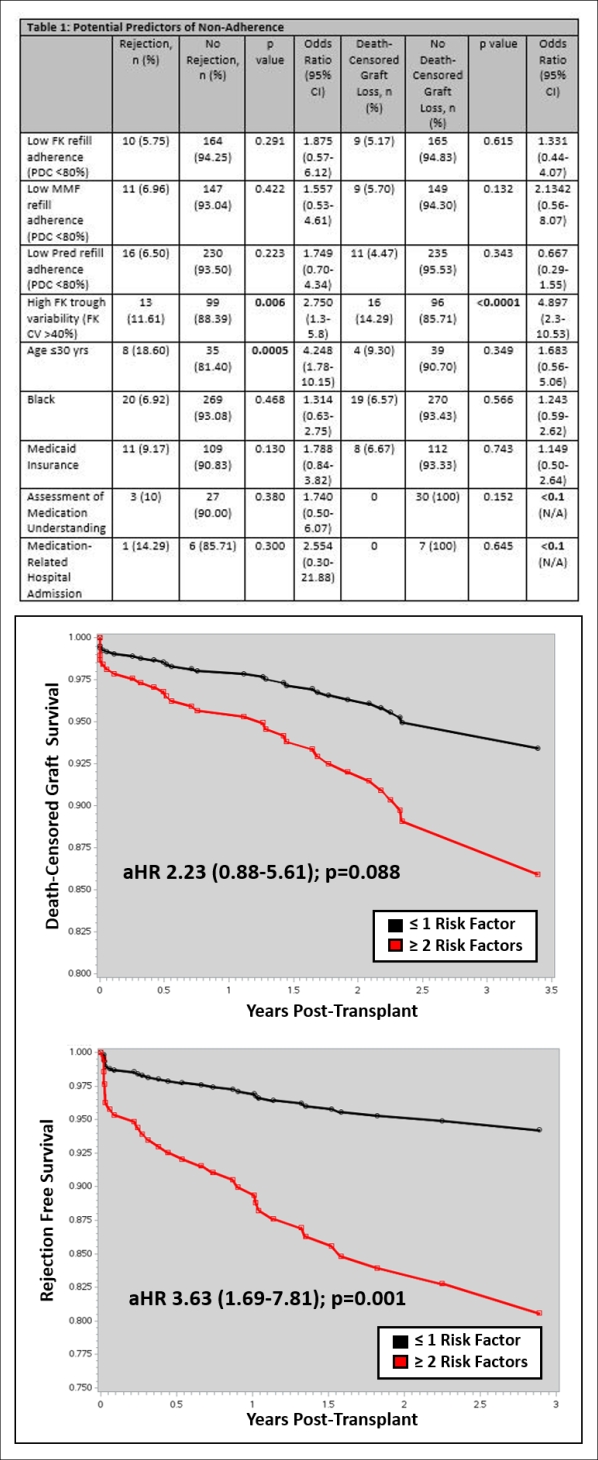
Methods: Retrospective longitudinal cohort study of KTRs between 1/2014 and 7/2017. We assessed 7 potential predictors for non-adherence: percentage of days covered (PDCs) of medications (refill adherence), high tacrolimus concentration variability (FK CV), age ≤30 years, race, insurance, pharmacist's assessment of patient's understanding of medication regimen at first clinic visit and medication-related problems resulting in readmission during the first year. PDC <80% was defined as low adherence and FK CV >40% was defined as high variability. These were validated using the outcomes of death-censored graft survival and rejection free survival.
Results: 513 KTRs were included. Four of the 7 potential predictors of non-adherence demonstrated association with outcomes, including high tacrolimus trough variability, younger age, Medicaid insurance and readmission for medication related problems. Immunosuppression refill adherence (PDC), AA race, and pharmacist's assessment of the patient's understanding of medication regimen were not associated with outcomes (Table 1). Based on this, patients were categorized as high risk if they had 2 or more of the 4 predictors of non-adherence. These patients were at a substantially higher risk of both acute rejection (Figure 1, aHR 3.63 (1.69-7.81); p=0.001) and death-censored graft loss (Figure 1, aHR 2.23 (0.88-5.61); p=0.088).
Conclusion: Traditional risk-factors for non-adherence, including immunosuppression refill adherence and AA race may not be predictive of graft outcomes in contemporary KTRs. However, tacrolimus variability, Medicaid insurance, younger age and medication related readmissions continue to be strongly associated with acute rejection and graft loss.
CITATION INFORMATION: Harrison T., Perez C., Patel N., Meadows H., Fleming J., Pilch N., O'Brien B., Corbo H., Hardcopf J., Baliga P., DuBay D., Taber D. Assessment and Validation of Potential Predictors of Non-Adherence in Contemporary Kidney Transplant Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Harrison T, Perez C, Patel N, Meadows H, Fleming J, Pilch N, O'Brien B, Corbo H, Hardcopf J, Baliga P, DuBay D, Taber D. Assessment and Validation of Potential Predictors of Non-Adherence in Contemporary Kidney Transplant Recipients [abstract]. https://atcmeetingabstracts.com/abstract/assessment-and-validation-of-potential-predictors-of-non-adherence-in-contemporary-kidney-transplant-recipients/. Accessed March 4, 2026.« Back to 2018 American Transplant Congress