Are Some “High-Risk” Renal Transplants Recipients Higher Risk Than Others?
The Methodist Hospital, Houston
Meeting: 2013 American Transplant Congress
Abstract number: C1347
In renal transplantation, African Americans (AA), and nonAA sensitized with >20% panel reactive antibodies (PRA) are commonly accepted as “high-risk” for rejection and thus routinely administered depleting induction and similar maintenance therapies. The purpose of this study was to determine the incidence of rejection and de novo donor specific antibodies (DSA) among subgroups of this population, stratified by age (> or <60) and race (AA or nonAA). Patients with pre-transplant DSA were excluded from the analysis. The cohort of 257 patients had a mean age of 48 years and consisted of 56% AA, 51% male, 75% deceased donor, 66% with PRA>20%, and 9% retransplants. All received rATG induction and tacrolimus, mycophenolate, and steroid maintenance. The mean dose of rATG (4.97 mg/kg) did not differ among subgroups. At a median follow-up was 28 months (range 2-80) the incidence of rejection ranged from 6-27% (fig.1). When further grouped by age only, rejection occurred in 7.2% of patients >60 years regardless of race or sensitization, compared to 21% in patients <60 (p=0.009). DSAs were monitored in 214 patients, and were found to be positive in 18-40% (fig.2). When grouped by race, AA were significantly more likely to develop DSA than nonAA (35% vs. 20%; p=0.015). Five-year graft survival was significantly worse in those with rejection compared to those without rejection (69% vs. 87%; p=0.024, log-rank), however no difference was seen in graft survival based on DSA detection (84% with vs. 86% without).
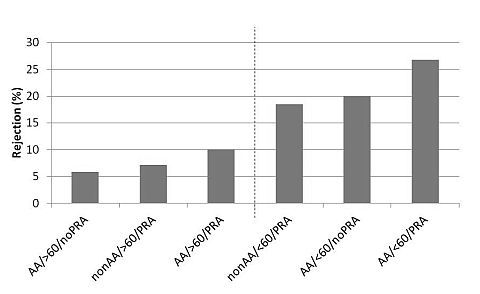
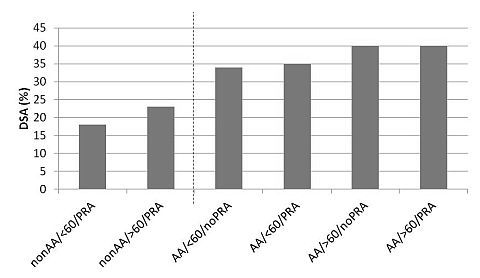
In this cohort of high-risk patients, a uniformly potent immunosuppressive strategy resulted in a nearly 5-fold variance in actual rejection rates and slight differences in DSA development. Rejection was associated with significantly worse 5-year graft survival. Application of a uniform immunosuppressive strategy in high-risk recipients does not result in a uniform incidence of acute rejection.
To cite this abstract in AMA style:
Patel S, DeVos J, Knight R, Gaber A. Are Some “High-Risk” Renal Transplants Recipients Higher Risk Than Others? [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/are-some-high-risk-renal-transplants-recipients-higher-risk-than-others/. Accessed February 27, 2026.« Back to 2013 American Transplant Congress
