An Improved Method for the Evaluation of Microvascular Inflammation in Renal Allograft Biopsies.
M. Rooney,1 Z. Ping,2 D. Samarapungavan,3 R. Hennigar.4
1Incyte Diagnostics, Spokane Valley, WA
2Pathology, Beaumont Hospitals, Royal Oak, MI
3Nephrology, Beaumont Hospitals, Royal Oak, MI
4Nephropathology Associates, Little Rock, AR.
Meeting: 2016 American Transplant Congress
Abstract number: 195
Keywords: Kidney transplantation, Perforin, Rejection
Session Information
Session Name: Concurrent Session: Identifying Antibodies - Tools of the Trade
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: Ballroom B
Background: Microvascular inflammation (MVI), assessed as glomerulitis (g) + peritubular capillaritis (ptc), is associated with T cell mediated (CMR) and antibody mediated (AMR) allograft rejection. It is a key finding in diagnosis of C4d-negative AMR. For that reason it was incorporated into the 2013 update of the Banff classification. There is high inter-observer variability however.
We observed a high proportion of MVI cells in allograft rejection are activated cytotoxic T cells with aggregated perforin-positive granules detectable by immunohistochemistry (IHC). Perforin positive cells are rare in the interstitium and tubules. In this setting the perforin stain is a stain for MVI. We sought to determine whether it could substitute for the calculation of MVI.
Design: Fifty clinically indicated renal allograft biopsies were selected to include various classes of rejection based on the 2013 Banff criteria. Perforin IHC was performed on each biopsy using a mouse monoclonal antibody, and the number of perforin positive cells per 10 high power fields (400X) was counted blindly and recorded.
Results: Table 1. Mean perforin positive cells per 10 high power fields (hpf) in renal transplant biopsies grouped by Banff classification.
| Classification of rejection: | No rejection | CMR 1a | CMR 1b | CMR 2a & 2b | AMR |
| n | 17 | 8 | 7 | 6 | 12 |
| Positive cells per 10 h.p.f. | 19.8 +/- 7.1 | 25.5 +/- 12.8 | 57.0 +/- 7.7 | 45.0 +/- 8.4 | 93.1 +/- 17.2 |
Cases of CMR graded at 1B or higher, and cases of AMR had increased perforin counts per unit area over cases with no acute rejection or CMR 1a (p<0.05). Cases of AMR had higher mean perforin counts than patients with either 1B or 2 ACR (p<0.05).
Conclusion: Perforin counts show the same associations with allograft rejection as previously shown for MVI. The perforin count stratifies patients into three risk groups: 1. no rejection and CMR 1a, 2. CMR 1b and 2, and 3. AMR.
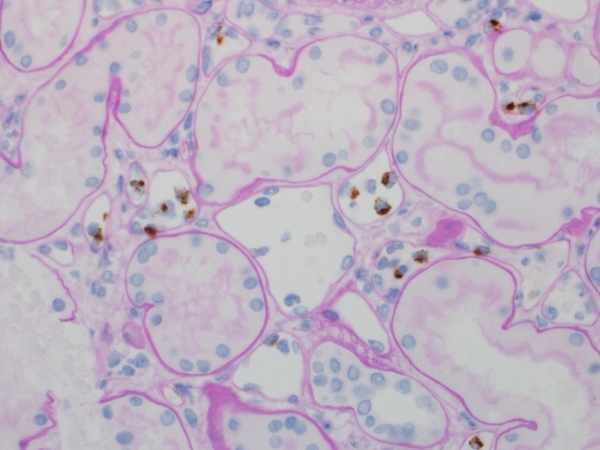
Perforin-positive lymphocytes in peritubular capillaries in an allograft biopsy (400X).
CITATION INFORMATION: Rooney M, Ping Z, Samarapungavan D, Hennigar R. An Improved Method for the Evaluation of Microvascular Inflammation in Renal Allograft Biopsies. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Rooney M, Ping Z, Samarapungavan D, Hennigar R. An Improved Method for the Evaluation of Microvascular Inflammation in Renal Allograft Biopsies. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/an-improved-method-for-the-evaluation-of-microvascular-inflammation-in-renal-allograft-biopsies/. Accessed February 18, 2026.« Back to 2016 American Transplant Congress
