An Assurance of Insurance: Should Living Kidney Donors Be Required to Have Health Insurance?
J. Siegel,1 A. Humar,2 P. Gianaros,1 J. Steel.2
1Department of Psychology, University of Pittsburgh, Pittsburgh, PA
2Department of Surgery, Division of Transplantation, University of Pittsburgh, Pittsburgh, PA.
Meeting: 2016 American Transplant Congress
Abstract number: C171
Keywords: Hypertension, Kidney transplantation, Psychosocial, Public policy
Session Information
Session Name: Poster Session C: Kidney Donor Evaluation and Donor Nephrectomy
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Lack of health insurance has been related lack of access to health care, poorer health, and increased mortality. In this study, we investigate sociodemographic predictors of insurance status in living kidney donors, examine reasons why patients were declined from surgery by insurance status, and tested if the health insurance status of donors is related to higher blood pressure pre- and post-surgery. We conducted a retrospective chart review of 680 consecutive patients evaluated for living kidney donation between January 2010 and June 2015. Sociodemographic medical and psychiatric factors were collected to assess the predictors of insurance reasons for being declined for surgery. Blood pressures were recorded prior to surgery and 6, 12, and 24 months. Mann Whitney U, Chi-square analyses, and logistic regression were performed to examine predictors of insurance status and declination for surgery. A mixed-model linear regression model then tested the predictors of changes in pre and post-blood pressures. Using logistic regression, significant predictors of insurance included higher levels of education [p = 0.007] and being married [p = 0.031]. Those without insurance were significantly more likely to be declined for psychosocial reasons than those with health insurance (p < 0.001). Follow-up rates for blood pressure were significantly lower for those without insurance at six months (43%) [p = 0.029] and one year (35%) [p < 0.001] than those with insurance (77%, 69%). 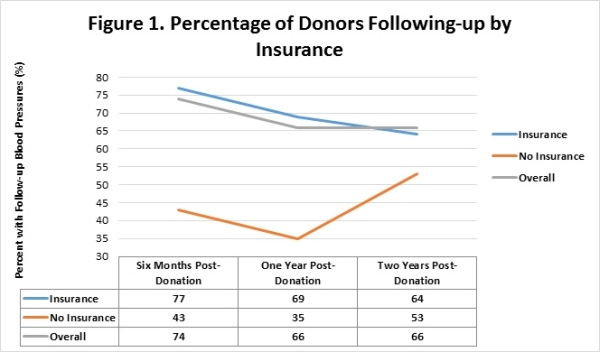 The mixed-model linear regression found significant predictors of systolic blood pressure included gender, [p< 0.001]; race [p = 0.012]; and age [p < 0.001], Significant predictors of diastolic blood pressure included gender [p < 0.001]; race [p = 0.020]; and drug use [p = 0.003]. Health insurance was predictive of systolic blood pressure but not statistically significant. The low rate of follow-up for those without insurance necessitates future research. Interventions for without insurance to increase follow-up rates may improve the health and safety of these donors.
The mixed-model linear regression found significant predictors of systolic blood pressure included gender, [p< 0.001]; race [p = 0.012]; and age [p < 0.001], Significant predictors of diastolic blood pressure included gender [p < 0.001]; race [p = 0.020]; and drug use [p = 0.003]. Health insurance was predictive of systolic blood pressure but not statistically significant. The low rate of follow-up for those without insurance necessitates future research. Interventions for without insurance to increase follow-up rates may improve the health and safety of these donors.
CITATION INFORMATION: Siegel J, Humar A, Gianaros P, Steel J. An Assurance of Insurance: Should Living Kidney Donors Be Required to Have Health Insurance? Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Siegel J, Humar A, Gianaros P, Steel J. An Assurance of Insurance: Should Living Kidney Donors Be Required to Have Health Insurance? [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/an-assurance-of-insurance-should-living-kidney-donors-be-required-to-have-health-insurance/. Accessed March 3, 2026.« Back to 2016 American Transplant Congress
