Ambulatory Blood Pressure Monitoring Detects High Prevalence of Hypertension in Recipients of Non-Renal Transplants.
1Dept. of Ped. Kidney, Liver and Metabolic Diseases, Hannover Medical School, Hannover, Germany
2Dept. of Ped. Hematology, Hannover Medical School, Hannover, Germany
3Dept. of Ped. Pulmonology, Hannover Medical School, Hannover, Germany
4Dept. of Nephrology, Hannover Medical School, Hannover, Germany
Meeting: 2017 American Transplant Congress
Abstract number: D159
Keywords: Arteriosclerosis, Hypertension, Morbidity, Pediatric
Session Information
Session Name: Poster Session D: Kidney: Pediatric
Session Type: Poster Session
Date: Tuesday, May 2, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Long-term survival after pediatric non-renal organ and stem cell transplantation (tx) has become increasingly better. The optimal post-transplant care therefore goes beyond organ-specific issues and also addresses patients' comorbidities. Hypertension (HTN) is a major, but modifiable cardiovascular risk factor. Our aim was to describe the prevalence of HTN in recipients of non-renal tx (lung, liver, stem cell) in comparison to kidney tx recipients.
We prospectively assessed 225 pediatric patients (54% male; mean age 13±4 years) after kidney (n=88), liver (n=54), lung (n=38), and stem cell (n=45) tx. Mean time after tx was 5±4 years. In addition to casual blood pressure (BP), we used ambulatory blood pressure monitoring (ABPM) to enable the diagnosis of masked HTN (normal casual BP, but elevated ABPM) and nocturnal HTN (normal daytime, but elevated nighttime ABPM).
As expected after kidney tx, HTN affected almost all patients (94%). Almost half of these patients had either uncontrolled (44%) or untreated (4%) HTN (Fig.1A). HTN was also highly prevalent in patients after lung (84%), liver (44%) and stem cell (24%) tx. The frequency of uncontrolled/untreated HTN was higher in the non-renal tx recipients (up to 91% in stem cell tx) when compared to kidney tx. Fig.1B and 1C depict the contribution of masked and nocturnal HTN.
Our analysis demonstrates the high prevalence of HTN in non-renal tx recipients and illustrates the importance of ABPM in diagnosing HTN in these patients. Up to 72% of hypertensive patients were only diagnosed by ABPM (lung: 13%; liver: 52%; stem cell: 72%). The high rate of insufficiently (uncontrolled) or even untreated patients demonstrates that further efforts are needed to improve patient care in order to prevent cardiovascular morbidity and mortality in adulthood.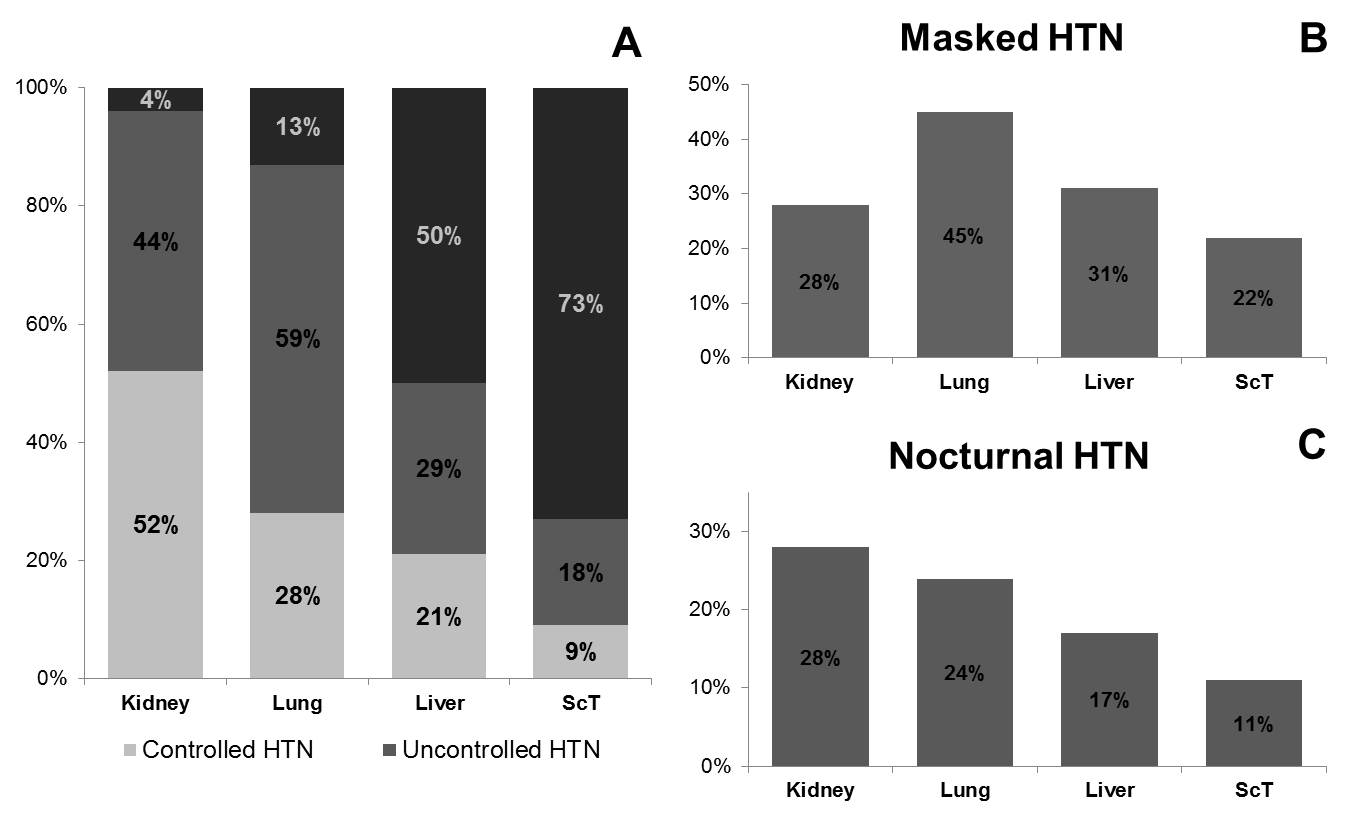
CITATION INFORMATION: Melk A, Memaran Dadgar N, Borchert-Mörlins B, Sugianto R, Blöte R, Goldschmidt I, Beier R, Müller C, Schmidt B. Ambulatory Blood Pressure Monitoring Detects High Prevalence of Hypertension in Recipients of Non-Renal Transplants. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Melk A, Dadgar NMemaran, Borchert-Mörlins B, Sugianto R, Blöte R, Goldschmidt I, Beier R, Müller C, Schmidt B. Ambulatory Blood Pressure Monitoring Detects High Prevalence of Hypertension in Recipients of Non-Renal Transplants. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/ambulatory-blood-pressure-monitoring-detects-high-prevalence-of-hypertension-in-recipients-of-non-renal-transplants/. Accessed February 22, 2026.« Back to 2017 American Transplant Congress
