Adult Living Donor vs. Deceased Donor Liver Transplant (LDLT vs. DDLT) at a Single US Center- Time to Change Our Paradigm for Liver Transplant
A. Humar, D. Jorgensen, S. Ganesh, A. Tevar, M. Molinari, C. Hughes
Thomas E Starzl Transplant Inst, Pittsburgh, PA
Meeting: 2019 American Transplant Congress
Abstract number: 458
Keywords: Living-related liver donors, Outcome
Session Information
Session Name: Concurrent Session: Liver: Living Donors and Partial Grafts
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: Room 312
*Purpose: LDLT remains underutilized in the US. We compared outcomes between LDLT and DDLT at our center to highlight the advantages of LDLT.
*Methods: Retrospective review of 226 adult LDLTs vs 632 DDLTs performed at a single center by a single team between 2009 to present.
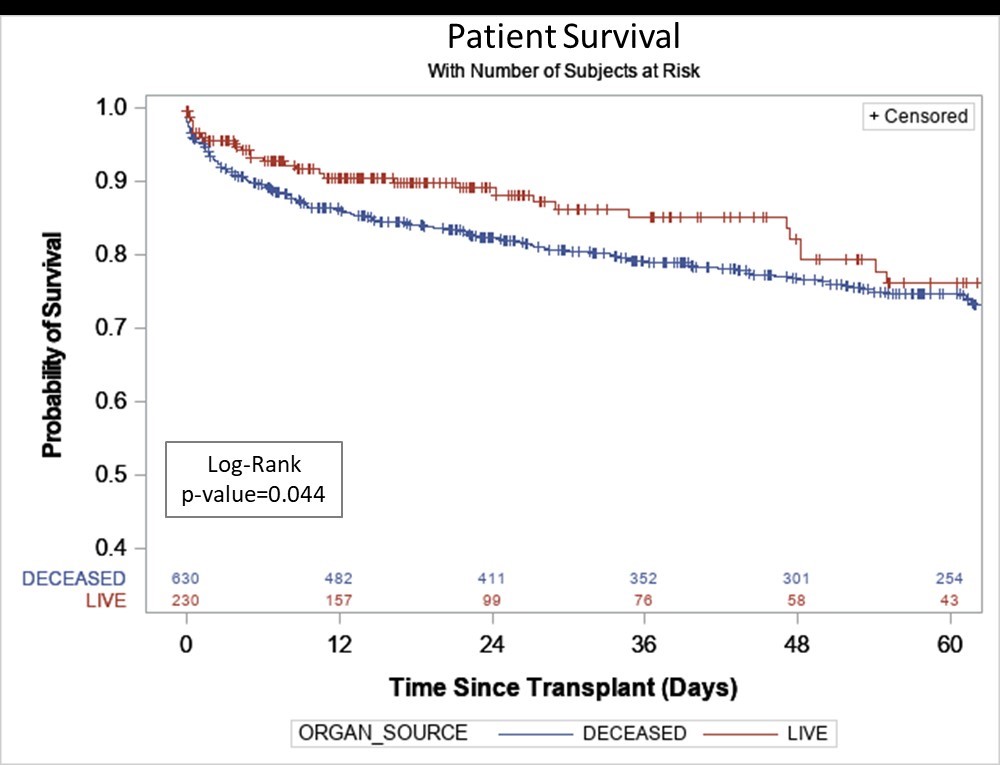
*Results: LDLT vs DDLT recipients were similar age (55.8 vs 55.8, p=0.99), race, and BMI (28.5 vs 29.5, p=0.12), but differed in donor age (36.6 vs 43.5, p<0.01), calculated MELD at transplant (23.3 vs 27.5, p<0.01) and median waiting time from listing to transplant (104 vs 146 days). DDLT patients had 2.7 admissions/yr to hospital while on waiting list. Overall, survival outcomes were superior in LDLT recipients (1-year 91% vs 86%, 3-year 86% vs 79%, p=0.04, Figure). Even in high risk subgroups such as retransplants or fulminant hepatic failure, results were equivalent or superior with LDLT. Other outcomes demonstrated shorter length of hospital stay in LDLT recipients (median 11 vs 14 days, p=0.02), less likelihood of intraoperative blood transfusion (52% vs 78%, p<0.01), overall less blood product use, and less likelihood of posttransplant dialysis. Early reoperation and biliary/vascular complication rates were similar between the 2 groups. Hospital charges related to the transplant itself were 30.8% lower for LDLT (p<0.01). Complications in living donors were acceptable with no early or late deaths, 3-month reoperation rate 3.1%, overall reoperation rate 5.7%, and overall complication rate 20.3%. Given advantages, we have expanded LDLT utilization at our center - in 2017, LDLT comprised 53.6% of our transplants (national average 4.5%), and our transplant rate increased from 44.8 in 2015 to 71.3 in 2017 (rate per 100 person years, SRTR data).
*Conclusions: LDLT offers advantages over DDLT including superior outcomes and less resource utilization. We feel it is time to change the paradigm of how LDLT is utilized in this country, offering it as the first choice in most cases rather than the last choice.
To cite this abstract in AMA style:
Humar A, Jorgensen D, Ganesh S, Tevar A, Molinari M, Hughes C. Adult Living Donor vs. Deceased Donor Liver Transplant (LDLT vs. DDLT) at a Single US Center- Time to Change Our Paradigm for Liver Transplant [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/adult-living-donor-vs-deceased-donor-liver-transplant-ldlt-vs-ddlt-at-a-single-us-center-time-to-change-our-paradigm-for-liver-transplant/. Accessed February 21, 2026.« Back to 2019 American Transplant Congress