A Psychosocial Clinician Rating Scale is Used Differently Across Solid Organ Teams within a Single Transplant Center
S. Entenman1, T. Chaffee2, M. Pienta3, B. Young3, E. Clifton1, J. Mellinger4, L. McElroy5, G. Winder1
1Psychiatry, University of Michigan, Ann Arbor, MI, 2Psychiatry, University of Missouri-Kansas City, Kansas City, MO, 3Surgery, University of Michigan, Ann Arbor, MI, 4Internal Medicine, University of Michigan, Ann Arbor, MI, 5Surgery, Duke University, Durham, NC
Meeting: 2021 American Transplant Congress
Abstract number: 707
Keywords: Psychiatric comorbidity, Psychosocial, Risk factors, Screening
Topic: Clinical Science » Ethics » Psychosocial and Treatment Adherence
Session Information
Session Name: Psychosocial and Treatment Adherence
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Transplant psychosocial clinician rating scales like the Stanford Integrated Psychosocial Assessment for Transplant (SIPAT) are widely used tools to standardize subjective patient data, stratify risk, supplement clinician decision-making, and facilitate research. Psychosocial clinicians within a single center often evaluate candidates and assign SIPAT scores across diverse transplant patient populations. The goal of this study was to describe how different solid organ teams use and apply the SIPAT despite the uniformity of the instrument’s criteria and interpretation. In 2015, Michigan Medicine deployed the SIPAT for use on all its solid organ transplant teams.
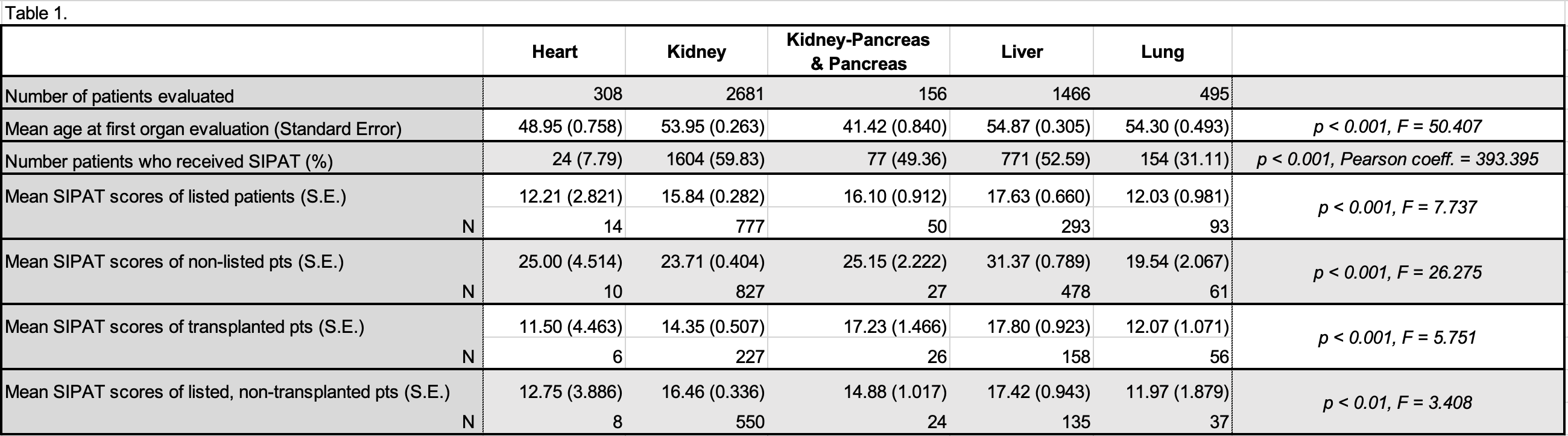
*Methods: Adult solid organ transplant candidates between 2015-18 were queried for SIPAT score at the time of transplant evaluation. For patients who were evaluated multiple times or for multiple organs, the first evaluation was used. Rates of SIPAT use were compared among the organ teams. SIPAT scores range in categories from excellent (0-6) to poor (> 70). Mean SIPAT scores were compared between listed, non-listed, transplanted and non-transplanted candidates. Chi-square tests were used for categorical data; ANOVA was used for continuous data.
*Results: A total of 5108 patients were evaluated during the study period. The majority of patients were male (60%), Caucasian (73.7%), and married (46.0%). Age at first evaluation varied significantly across organs. 2630 of 5106 (51.5%) patients received a SIPAT score, with scores ranging from 0 to 87. Kidney and liver were the most avid SIPAT users followed by kidney-pancreas and pancreas, lung, and heart (see Table 1). Mean scores of listed, non-listed, transplanted, and non-transplanted patients, were all statistically different across the organ teams. Intuitively, SIPAT scores trended higher for non-listed and non-transplanted patients.
*Conclusions: These cross-organ differences in SIPAT frequency and mean scores are relevant to all psychosocial clinicians, particularly those evaluating candidates for separate organs and interacting with different transplant teams.
To cite this abstract in AMA style:
Entenman S, Chaffee T, Pienta M, Young B, Clifton E, Mellinger J, McElroy L, Winder G. A Psychosocial Clinician Rating Scale is Used Differently Across Solid Organ Teams within a Single Transplant Center [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/a-psychosocial-clinician-rating-scale-is-used-differently-across-solid-organ-teams-within-a-single-transplant-center/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress